general information
A professional organization, which is the Respiratory Society of Russia, unites doctors involved in the field of pulmonology. Detailed developments on the diagnosis and treatment of pneumonia, occurring in various forms and taking into account the severity of the disease, formed the basis of recommendations that allow a differentiated approach to:
- the appointment of a diagnostic minimum;
- choosing the most effective antibacterial drugs;
- making a decision on the advisability of inpatient or outpatient treatment.
Classification of pathology
Pneumonia is dangerous disease, in which hospital treatment is often required due to the serious condition of the patient, accompanied by signs of intoxication, high fever, intense cough, and general weakness. However, the manifestation is not always inflammatory process in the lungs proceeds in such an expressive form.
Considering the forms of manifestation of the disease, criteria were developed that distinguish the following types of pathology:
- community-acquired pneumonia. She is out-of-hospital, home or outpatient. This is the most common option. The route of infection is communication with carriers of pathogens (pneumococci, staphylococci, chlamydia and Pseudomonas aeruginosa). This form of pneumonia affects the lower parts of the organ.
- Hospital (nosocomial or nosocomial). Clinical signs more expressive, treatment requires mandatory hospitalization.
- Aspiration. The causative agent of the disease is several types of bacteria.
The classification also provides for the allocation of the following varieties, taking into account the localization of the pathological process:
- right-sided pneumonia;
- left-sided;
- bilateral.
According to the growth of the inflammatory process, the following types of pathology are distinguished:
- focal pneumonia - there is a lesion of a small area of \u200b\u200bthe lung;
- segmental - there are several foci;
- totalitarian - inflammation covers the entire lung or two at once.
According to the severity of the clinical picture, pneumonia is mild, moderate or severe form.
Depending on the patient's condition, an individual treatment tactic is chosen, which allows outpatient treatment under the constant supervision of a doctor.
SARS
This type of disease belongs to the out-of-hospital category. Its features clinical course formed the basis of the name. Among characteristic manifestations at the beginning of the disease, there are symptoms inherent in ARVI or the common cold - malaise, aching joints, nasal congestion. Then other symptoms appear:
- chills;
- runny nose;
- unproductive cough;
- wheezing in the lungs is practically not audible;
- leukocytes increase in rare cases;
- the main pathogens are mycoplasmas, legionella, chlamydia.
- Clarithromycin;
- Erythromycin;
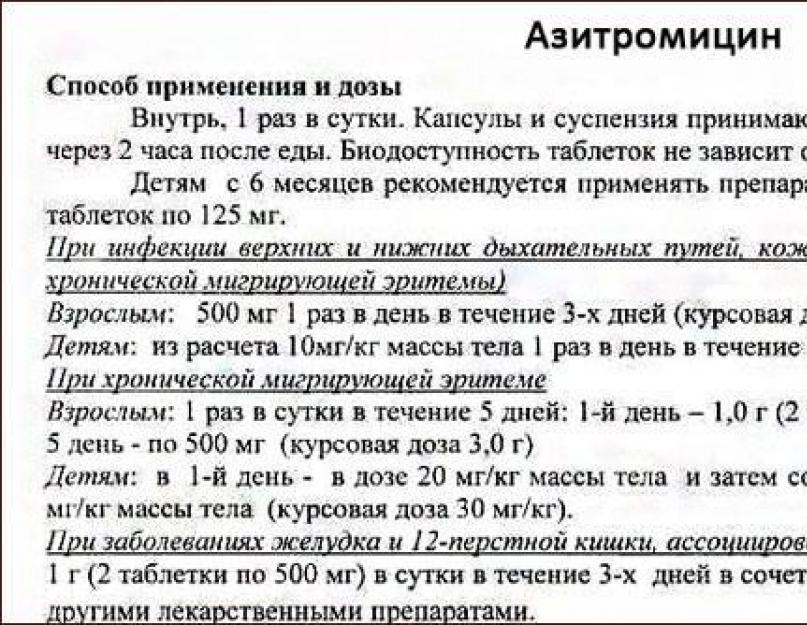
- Azithromycin;
- doxycycline;
- Levofloxacin.

Data medical preparations effective in resisting disease-causing agents. Positive dynamics of treatment is observed within 24-48 hours. However, the full course of therapy is 10-12 days.
Community-acquired pneumonia in children
At this age, this type of disease is observed very often. Clinical signs of pathology are somewhat different from the manifestations characteristic of elderly patients. Increased irritability and excitability is characteristic of young patients, while confusion may occur in older patients.
In addition, all other symptoms (they are mentioned above) in children are more intense and expressive, which served as the basis for the development of clinical guidelines regarding the direct treatment of pediatric community-acquired pneumonia.
Russian experts substantiate their point of view by the likelihood of developing complications from incorrect treatment, which can have a more negative impact on the child's body than a small dose of radiation.
Particular attention is paid to the use of antibiotic therapy.. It is recommended to consider the following factors:
- sensitivity of identified pathogens to a certain number of antibiotics;
- age of a small patient;
- the presence of a history of concomitant diseases;
- previous antibiotics.
High demands are placed on the criteria for the effectiveness of the treatment of pneumonia in children. They provide for the onset of positive dynamics in the child's condition on the 2nd-3rd day of therapy and the final recovery after 6-12 days.
Federal developments provide, in addition to examining and listening to the patient, the mandatory implementation of the following diagnostic procedures:
- x-rays to confirm the diagnosis;
- clinical examination of blood;
- biochemical tests to detect the level of transaminase, creatinine, urea, electrolytes.
Such a minimum of samples is carried out with a mild course of the disease, allowing an outpatient course of therapy.
Identification of moderate and severe pneumonia involves the mandatory hospitalization of the patient and more in-depth diagnostic tests. Among them:
- sputum culture to identify the type of infectious agent in order to determine sensitivity to antibiotics;
- smear microscopy (according to Gram);
- blood biochemistry;
- chest CT;
- blood gas test.
The last test is carried out in a severe form of the pathological condition.
The presence of a pleural effusion associated with painful sensations in the chest area and shortness of breath, is an indication for a puncture.
The results of the examination become decisive for the diagnosis, the conclusion about the possibility of outpatient treatment or the need for a treatment course in a hospital setting.
The fundamental principle of the therapeutic effect on the focus of inflammation is the use of antibacterial drugs, taking into account a differentiated approach to the impact on various types of pathology, as well as - age features and the patient's condition
- Outpatient treatment for community-acquired pneumonia involves the use of antibiotics penicillin series in tablets or capsules. Amoxicillin is recommended. If a chlamydial pathogen or intolerance to penicillin is detected, macrolides are prescribed - Azithromycin or Clarithromycin. The lack of effectiveness of therapy allows their replacement with fluoroquinolones. The most effective drug from this group is Levofloxacin.
- The severe course of the pathology becomes an indication for mandatory treatment in a hospital. The main requirement of the recommendations is the use of combinations, including a penicillin antibiotic and macrolytics or cephalosporins. The drugs are administered mainly intravenously. The following combinations are used: a macrolide drug in combination with Amoxiclav or a macrolide with Ceftriaxone.
- The presence of concomitant diseases in patients over 60 years of age (diabetes, dystrophy, alcoholism, liver cirrhosis or renal failure) is an indication for the appointment of Amoxiclav (aminopenicillin group) or Cefuroxime (from cephalosporins). Alternatively, fluoroquinolones should be given. Depending on the severity of the pathology, therapy is carried out with a tablet course or injection of drugs.
- Clinical guidelines for pneumonia in children also allow the use of antibiotics in tablets and capsules for mild illness. Pneumonia of moderate and severe form is an indication for the use of an intramuscular or intravenous method of administering drugs. If a history of previous antibiotics was present, it is recommended to prescribe Amoxiclav or cephalosporins. Diagnosis of mycoplasmal and chlamydial etiology of the disease involves the appointment of macrolide drugs.

The criteria for the effectiveness of therapy are determined by decreasing clinical signs - easier breathing, absence of fever and signs of intoxication, stabilization of temperature indicators. With adequate treatment, positive dynamics is observed in the first three days. Its absence during this period becomes an indication for changing the therapeutic course regimen.
The use of the studied experience greatly contributes to the effectiveness of therapy in outpatient and inpatient treatment of pneumonia.
The respiratory system performs one of the most important functions in our body. It provides cells, organs and tissues with uninterrupted breathing and the removal of harmful carbon dioxide from them. Inflammatory diseases lungs greatly reduces respiratory function, and such a pathology as community-acquired pneumonia can lead to deep respiratory failure, oxygen starvation of the brain and severe complications.
Community-acquired pneumonia is called pneumonia, which struck a person outside medical institution or within 48 hours of admission to the hospital.
Characteristic symptoms
Inflammation of the lung structures begins acutely. There are several criteria that should alert the environment of a sick person and contribute to his coming to the doctor:
- a state of fever;
- cough;
- dyspnea;
- chest pain.
This set of symptoms should be a signal to go to the clinic to see a doctor.
Fever is manifested by chills, headache, temperature rise to high numbers. Possible nausea, vomiting after eating, dizziness. In severe cases, convulsive readiness, a state of confused consciousness.
Cough, dry at first, painful. After a few days, the sputum begins to move away. It can be of various consistency: from mucous to purulent with streaks of blood. Shortness of breath with pathologies of breathing of the expiratory (on exhalation) type. Pain are of different intensities.
Very rarely, in old age there may be no fever. This happens after the age of 60, in 25% of all pneumonias. The disease manifests itself with other symptoms. Chronic diseases come to the fore. There is weakness, severe fatigue. Abdominal pain, nausea are possible. Elderly people often lead a reclusive and sedentary lifestyle, which contributes to the development of congestion in the lungs and clinically atypical forms of pneumonia.
Main reasons
A healthy body is protected from most pathogenic microbes and pneumonia is not dangerous for it. But when unfavorable conditions arise, the risk of disease increases. The most common factors that can lead to pneumonia are:
- tobacco smoking;
- viral diseases of the upper respiratory tract;
- chronic pathologies of the heart, gastrointestinal tract, kidneys and liver;
- contacts with wild animals, birds, rodents;
- frequent changes of residence (travel to other countries);
- systematic or one-time severe hypothermia;
- junior and elderly age(unlike adults, children and the elderly get sick more often).

Predisposing factors often become the trigger of the disease, but community-acquired pneumonia occurs only if the pathogen has entered the lungs.
Classification of types of pathogens in percentage terms
| Pathogen | % | Characteristic |
| Pneumococcus | 30–40 | The main causative agent of pneumonia. |
| Mycoplasma | 15–20 | Causes atypical inflammation in the lung tissue. |
| Haemophilus influenzae | 3–10 | Pneumonia caused by this bacterium is most prone to purulent complications. |
| Staphylococcus aureus | 2–5 | Lives on the mucous membranes of most people, affects weakened organisms. |
| Influenza viruses | 7 | Cause specific viral inflammation of the lungs. |
| Chlamydia | 2–8 | It mainly causes diseases of the genital organs in humans, but is also carried by rodents and birds, so it can sometimes cause pneumonia. |
| Legionella | 2–10 | It is the causative agent of "legionnaires' disease" and Pontiac fever, sometimes causing pneumonia. Can safely live and breed in many environments. |
| Other flora | 2–10 | Klebsiella, Pseudomonas aeruginosa and Escherichia coli, Proteus, other microorganisms. |
Basically, the infection enters the body in three ways:
- Transbronchial, through the respiratory system, with air flow from outside.
- Contact, that is, direct contact of the infected substrate with lung tissue.
- Hematogenous, from the primary focus with blood flow through the vessels.
Diagnostics
Upon admission of a patient with suspected pneumonia, the doctor begins the diagnosis with a survey of complaints and an initial examination with physical examination methods:

- palpation;
- percussion;
- listening.
When tapping, the sound is shortened over the affected part of the lung, the greater the dullness, the higher the risk of detecting complications. Auscultation shows localized bronchial breathing, wheezing of various calibers, possibly crepitus. Palpation of the chest reveals increased bronchophony and voice trembling.
- chest x-ray;
- general analysis blood.
Performed in the hospital biochemical analysis blood, sputum examination for the presence of microflora. A complete blood count shows signs of inflammation:
- leukocytosis, with a shift of the formula to the left;
- increased ESR;
- sometimes toxic erythrocyte granularity and aneosinophilia.

On the radiograph, a sign of pneumonia is an infiltrative darkening of the lung tissue, which can be of different sizes, from focal to total (right / left-sided) and bilateral. At unusual picture on the radiograph (incomprehensible changes or “nothing” in the lungs), computed tomography is prescribed for a more complete visualization of the lesions.
Clinical guidelines for the diagnosis of community-acquired pneumonia indicate several clinical and laboratory signs for the detection of severe pneumonia, in which the patient is shown hospitalization not in a specialized (therapeutic, pulmonological) hospital, but in the intensive care unit and intensive care.
Signs of severe pneumonia
| Clinical | Laboratory |
| Acute respiratory failure (Respiratory rate over 30 per minute). | A decrease in leukocyte blood count below 4. |
| Pressure less than 90/60 (in the absence of blood loss). | Damage to several lobes of the lungs on x-ray. |
| Decreased oxygen saturation below 90%. | Hemoglobin below 100 g/l. |
| Partial pressure in arterial blood below 60 mm. rt. Art. | |
| Confused state of consciousness, not associated with other diseases. | |
| Acute symptoms kidney failure. |
Any of these signs is a significant signal for a doctor to make a decision about hospitalizing a patient in an emergency department and starting a comprehensive therapy to restore the body.
Healing procedures
The general principles of inpatient treatment of community-acquired pneumonia are based on several important points:

- Gentle treatment for the patient.
- Complete drug therapy.
The regimen is chosen by the doctor depending on the clinical manifestations. In a feverish period - bed rest, with a raised headboard and frequent turns in bed. The patient is then allowed to walk a little.
Complex nutrition includes easily digestible carbohydrates, natural vitamins. The consumption of large volumes of liquid is mandatory.
Medical treatment consists of 3 main points:
- etiotropic therapy aimed at suppressing the pathogen (antibiotics, specific sera, immunoglobulins);
- detoxification therapy, which is aimed at reducing the level of fever, removing toxins from the body;
- symptomatic therapy.
Much attention is paid to the choice of antibiotic. Until the microflora is clarified, patients with pneumonia are treated empirically with antibiotics based on the following data:
- conditions for the occurrence of pneumonia;
- patient's age;
- the presence of concomitant pathologies;
- the severity of the disease.

The doctor chooses antibiotics a wide range actions (penicillins, cephalosporins). If the effect of treatment is absent within 2-4 days, the antibiotic is replaced with another one or the dose is increased. And after identifying the pathogen, etiotropic therapy is often corrected to increase efficiency.
The prognosis is favorable in the absence of severe pulmonary and other complications associated with chronic diseases. For effective recovery, timely access to a specialist is important. With inpatient treatment, an extract home is usually given after 2 weeks in the hospital.
An early visit to a consultation at a medical facility will allow the patient to be treated as an outpatient and take medications in a more comfortable home environment. However, when treating at home, it is necessary to observe a special regimen for the patient (separate dishes, mask regimen).
Prevention
Preventive measures aimed at reducing the risk of community-acquired pneumonia in the home should be carried out at different levels.
Prevention at the household level
Sanitary alertness in large groups
The management of enterprises should take care of labor protection, improve the technologies for performing work and industrial sanitation.
Public prevention
Mass sports campaign for healthy lifestyle life and the rejection of bad habits.
Prevention in medicine
Systematic timely vaccination of the population against influenza. The vaccine must correspond to the strain of the virus that progresses during the season of its use.
Personal prevention
Rational hardening, reducing the number of hypothermia (especially in the cold season), eliminating bad habits, daily sports.
Any disease is easier to prevent than to treat.
Pneumonia, or pneumonia, is a serious illnesses. It often requires hospitalization. Without adequate treatment with such a diagnosis, the patient may die.
Inflammation of the lungs can affect both the newborn and the elderly. Sometimes the pathology develops against the background of SARS, influenza, bronchitis - as a complication. But often it is an independent disease.
Pneumonia can be caused by a wide variety of bacteria, viruses, and even fungi. Often it proceeds violently, with severe symptoms and intoxication, however, an erased course of the disease also occurs.
Since the prognosis for the health and life of the patient depends on adequate treatment, the Russian Respiratory Society has developed national or federal clinical guidelines for the diagnosis and treatment of this disease.
Russian Respiratory Society
The Russian Respiratory Society is a professional medical organization including pulmonologists. There are similar societies in other countries - American Thoracic in the USA, British Thoracic and European Respiratory in Europe.
One of their most significant tasks is the development of clinical guidelines for the treatment of a particular disease. For the first time such recommendations were published in 1995 - on therapy bronchial asthma followed by chronic obstructive pulmonary disease.
Many specialists of the pulmonological profile of the Russian Federation took part in their development, and Chuchalin A.G., professor, doctor of medical sciences, academician of the Russian Academy of Medical Sciences, acted as the chief editor.
Definition

Pneumonia is an acute lesion of the lung tissue, which is accompanied by signs of infection in the lower respiratory tract and is confirmed by x-ray.
Typical symptoms of pneumonia include:
- Fever.
- Manifestations of intoxication (headache, vomiting, feeling unwell).
- Cough with expectoration, sometimes dry.
- Shortness of breath.
- Pain in the chest.
When x-rays in the picture will be determined by the foci of infiltration.
There are several classifications of pneumonia. Since the pathogen in most cases cannot be determined, it is customary to distinguish pathology by place and method of occurrence.
Pneumonia happens:
- Out-of-hospital, or home (most common).
- Hospital (intrahospital, nosocomial). It is usually more severe and difficult to treat.
- Aspiration. This form is often caused by an association of microbes.
- In persons with severe immunodeficiency (HIV, immunosuppressive therapy). Has a poor prognosis.

A doctor of any specialty is obliged to suspect the diagnosis in the aggregate characteristic symptoms and data objective examination. These include:
- Shortening of percussion sound in the focus of infiltration.
- The appearance of wet rales or crepitus.
- Bronchial breathing in an atypical place.
However, such a diagnosis can be made only after radiological confirmation.
Sometimes there is no opportunity for x-rays. If, at the same time, the examination data testify in favor of pneumonia, we can talk about an inaccurate or unconfirmed diagnosis.
If objective and radiological signs of pneumonia are not determined, the diagnosis is considered unlikely. In addition, there are laboratory methods examinations.
Laboratory methods
If a mild pneumonia or moderate, and the patient is treated on an outpatient basis, he must be prescribed the following tests:
- General blood analysis.
- Biochemical blood test (determination of transaminases, urea and creatinine, electrolytes). This analysis is carried out whenever possible.
Microbiological diagnostics as a routine method is not carried out due to inappropriateness.
- When a patient is admitted to a hospital, in addition to the above studies, they perform:
- Sputum smear microscopy, Gram-stained.
- Sputum culture with determination of its sensitivity to antibacterial drugs.
- Study of blood culture (venous blood).
- Determination of the gas composition of the blood. This is shown at severe forms to resolve the issue of the need for IVL.
If there is an effusion, the patient is given a pleural puncture to clarify the diagnosis.
You should be aware that in the treatment of pneumonia, non-drug methods (physiotherapy) do not have a pronounced effectiveness, and their appointment is impractical. The only exception is breathing exercises, but with a certain amount of sputum secreted.
The mainstay of treatment for pneumonia is antibiotics. The drug is selected taking into account the clinical form of the disease.
Thus, outpatients with community-acquired pneumonia - according to federal guidelines– start treatment with oral antibiotics (tablets and capsules).
First-line drugs are the penicillin group (amoxicillin) and macrolides (clarithromycin, azithromycin). The latter are prescribed for suspected chlamydial etiology of the disease, as well as for allergies to penicillin.
An alternative to these drugs (if intolerant or ineffective) are fluoroquinolones (levofloxacin).
In elderly patients (over 60 years of age), as well as in the presence of concomitant pathology, therapy begins with aminopenicillins (amoxiclav) or cephalosporins (cefuroxime). Fluoroquinolones are also an alternative in such patients.
Diseases that aggravate the course of pneumonia and worsen the prognosis are:
- Heart failure.
- Diabetes.
- Oncopathology.
- Physical exhaustion, dystrophy.
- Alcoholism and drug addiction.
- Chronic liver and kidney failure, cirrhosis of the liver.
Despite the comorbidity, the treatment of pneumonia in such patients can also be carried out in tablet forms.
Treatment of severe pneumonia

Severe forms of pneumonia require hospitalization of patients in a hospital for a detailed examination and constant medical supervision.
Antibacterial therapy in such a situation is carried out parenterally - drugs are administered intravenously. Usually, the combinations "amoxiclav + macrolide" or "ceftriaxone + macrolide" are used. The name of the antibiotic may change - depending on the prescription of the doctor, however, according to national guidelines this should be the simultaneous administration of drugs of the penicillin group or cephalosporins and macrolides.
Upon reaching clinical effect, positive dynamics after 3-5 days, you can transfer the patient to tablet forms of drugs.
Performance criteria
The effectiveness of the treatment for pneumonia is evaluated on the second or third day. First of all, pay attention to the following indicators:
- fever
- intoxication;
- breath.
The patient should reduce hyperthermia to subfebrile condition or even complete normalization. Symptoms of intoxication proper treatment decrease significantly, and respiratory failure is absent or mild.
In severe forms, the dynamics is not always so fast, but it should be positive by the end of the third day.
If there is no improvement after 72 hours, the antibiotic regimen is changed. With adequate antibiotic treatment, its duration is 7-10 days.
SARS

Despite the fact that SARS is essentially community-acquired, it has received a special name due to its clinical presentation. This form of the disease is characterized by the following features:
- It is more common in young patients.
- The beginning is similar to a cold or SARS (runny nose, weakness, muscle pain).
- The fever is moderate.
- Dry cough.
- Percussion and auscultation data are uninformative.
- In many cases, there is no leukocytosis in the general blood test.
The list of causative agents of this pathology is extensive. However, most often these are the following microorganisms:
- Chlamydia.
- Mycoplasmas.
- Legionella.
Therapy for SARS
- Macrolides (erythromycin, clarithromycin, azithromycin).
- Tetracyclines (doxycycline).
- Respiratory fluoroquinolones (levofloxacin).
At mild form it is acceptable to start treatment with tablets or capsules, but severe pneumonia requires only injection of antibiotics.
The criteria for the effectiveness of treatment are the same as for ordinary pneumonia. The duration of treatment is usually longer and ranges from 12-14 days.
Community-acquired pneumonia in children

Inflammation in the lungs childhood occurs quite often. The Russian Respiratory Society, together with the Interregional Pediatric Respiratory Society and the Federation of Pediatricians of the CIS countries, developed separate clinical guidelines for young patients.
Diagnosis of this pathology in this age group has its own characteristics. Foreign guidelines do not consider it appropriate to perform x-rays for all children with suspected community acquired pneumonia unless for health reasons they require hospitalization.
Solidarity with them and the "Standard of primary health care", which was developed and approved in 2012.
However, according to most Russian experts, the suspicion of pneumonia is the basis for performing x-rays, since untimely therapy can do more harm than the received radiation dose.
When uninformative x-ray the child may be recommended computed tomography of the chest.

The choice of antibiotic for community-acquired pneumonia in children is determined by many factors. These include the sensitivity of a possible pathogen, the age of the child, concomitant diseases, previous antibacterial treatment.
In mild and moderate forms, therapy begins with amoxicillin tablets. Dispersible tablets are preferred due to their higher bioavailability.
Children with underlying pathologies, as well as those who have recently taken antibiotics, are shown amoxiclav or second-generation cephalosporins.
In severe pneumonia, drugs are administered intramuscularly or intravenously.
If patients have signs of chlamydial or mycoplasmal pneumonia, it is advisable to start therapy with macrolides.
The duration of treatment for this disease in children can vary from 7 to 14 days, depending on the pathogen.
Agreed and approved by the Russian Society of Neonatologists based on the results of a collective discussion of the draft clinical guidelines.
Working group
Antonov Albert Grigorievich - Doctor of Medical Sciences, Professor, Chief Researcher of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Professor of the Department of Neonatology of the Federal State Autonomous Educational Institution of Higher Education "First Moscow State medical University them. THEM. Sechenov" of the Ministry of Health of Russia
Baybarina Elena Nikolaevna - Doctor of Medical Sciences, Professor, Chief Researcher of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow
Balashova Ekaterina Nikolaevna - Candidate of Medical Sciences, Head of Clinical Work at the Department of Resuscitation and Intensive Care of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow
Degtyarev Dmitry Nikolaevich - Doctor of Medical Sciences, Professor, Deputy Director for scientific work FSBI "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Head of the Department of Neonatology, FGAEI HE "First Moscow State Medical University named after I.I. THEM. Sechenov" of the Ministry of Health of Russia, Chairman of the Council of the Russian Society of Neonatologists
Zubkov Viktor Vasilyevich - Doctor of Medical Sciences, Head of the Department of Neonatology and Pediatrics, National Medical Research Center for Obstetrics, Gynecology and Perinatology. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Professor of the Department of Neonatology, FGAEI HE "First Moscow State Medical University named after I.I. THEM. Sechenov” of the Ministry of Health of Russia, Moscow
Ivanov Dmitry Olegovich - Doctor of Medical Sciences, Professor, Chief Freelance Specialist of the Ministry of Health of Russia in Neonatology, Acting Rector of the St. Petersburg State Pediatric Medical University of the Ministry of Health of Russia, member of the Russian Association of Perinatal Medicine Specialists, St. Petersburg
Ionov Oleg Vadimovich - Candidate of Medical Sciences, Head of the Department of Resuscitation and Intensive Care of the Department of Neonatology and Pediatrics of the Federal State Budgetary Institution National Medical Research Center for Obstetrics, Gynecology and Perinatology. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Associate Professor of the Department of Neonatology, FGAEI HE "First Moscow State Medical University. THEM. Sechenov" of the Ministry of Health of Russia
Karpova Anna Lvovna - Candidate of Medical Sciences, Deputy Chief Physician for Childhood, State Budgetary Institution of Healthcare of the Kaluga Region "Kaluga Regional clinical Hospital- Perinatal Center", chief neonatologist of the Kaluga region, Kaluga
Kirtbaya Anna Revazievna - Candidate of Medical Sciences, Head of Clinical Work at the Department of Resuscitation and Intensive Care of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Associate Professor of the Department of Neonatology, FGAEI HE "First Moscow State Medical University. THEM. Sechenov" of the Ministry of Health of Russia
Krokhina Ksenia Nikolaevna - Candidate of Medical Sciences, Senior Researcher at the Department of Resuscitation and Intensive Care of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow
Kryuchko Daria Sergeevna - Doctor of Medical Sciences, Head of the Department for Analysis and Coordination of Work on Improving the medical care, Associate Professor of the Department of Obstetrics, Gynecology, Neonatology, Anesthesiology and Resuscitation, Federal State Budgetary Institution “National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.N. acad. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow
Lenyushkina Anna Alekseevna - Ph.D. acad. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow
Li Alexander Georgievich - resuscitator, head of the department of resuscitation and intensive care of newborns of the Perinatal Center of the St. Petersburg State Pediatric Medical University of the Ministry of Health of Russia
Malyutina Lyudmila Vyacheslavovna - Candidate of Medical Sciences, Head of the Department of Resuscitation and Intensive Care for Newborns and Premature Babies, State Budgetary Institution of Health of the Moscow Region "Moscow Regional Perinatal Center", Moscow Region, Balashikha
Mebelova Inessa Isaakovna - Candidate of Medical Sciences, Head of the Neonatal Center of the Children's Republican Hospital, Chief Neonatologist of the Republic of Karelia, Petrozavodsk
Nikitina Irina Vladimirovna - Candidate of Medical Sciences, Senior Researcher of the Department of Resuscitation and Intensive Care of the Federal State Budgetary Institution "National Medical Research Center for Obstetrics, Gynecology and Perinatology named after N.I. acad. IN AND. Kulakov, Russia, Moscow
Petrenko Yury Valentinovich - chief neonatologist of the North-Western Federal District of Russia, vice-rector for medical work of the St. Petersburg State Pediatric Medical University of the Ministry of Health of the Russian Federation Ryndin Andrey Yu. Research Center for Obstetrics, Gynecology and Perinatology acad. IN AND. Kulakov" of the Ministry of Health of Russia, Associate Professor of the Department of Neonatology, FGAEI HE "First Moscow State Medical University. THEM. Sechenov" of the Ministry of Health of Russia
Ryumina Irina Ivanovna - Doctor of Medical Sciences, Head of the Department of Pathology of Newborns and Premature Babies, Federal State Budgetary Institution National Medical Research Center for Obstetrics, Gynecology and Perinatology. acad. IN AND. Kulakov" of the Ministry of Health of Russia, Professor of the Department of Neonatology, FGAEI HE "First Moscow State Medical University named after I.I. THEM. Sechenov" of the Ministry of Health of Russia
Romanenko Vladislav Alexandrovich - Doctor of Medical Sciences, Professor of the Department of Pediatrics, Institute of Additional vocational education Federal State Budgetary Educational Institution of Higher Education "South Ural State Medical University" of the Ministry of Health of Russia, Chelyabinsk
Abbreviations
ABT - antibacterial therapy
BPD - bronchopulmonary dysplasia
BP - anhydrous gap
VAP - ventilator-associated pneumonia
IVH - intraventricular hemorrhage
HFOV - high-frequency oscillatory lung ventilation
IVL - artificial lung ventilation
UTI - infection urinary tract
KOS - acid-base state
CTG - fetal cardiotocogram
NI - neutrophil index
NSG - neurosonography
KLA - complete blood count
OAM - general urinalysis
VLBW - very low body weight
NICU - intensive care unit, intensive care unit
newborns
ORS - open resuscitation system
ICU - intensive care unit
PCT - procalcitonin test (acute phase protein
inflammation)
RDS - respiratory distress syndrome
RCT - randomized controlled trial
SRP - C-reactive protein(acute phase protein)
GBS - group B streptococcus
PCR - polymerase chain reaction
ECG - electrocardiography
ELBW - extremely low body weight
EchoCG - echocardiography
INSURE (INtubate-SURfactant - Extubate) - intubation -
surfactant administration - extubation and transfer to
non-invasive respiratory therapy
Fi02 - fraction of oxygen in the inhaled gas mixture
Peep - peak pressure at the end of exhalation
Pip - peak inspiratory pressure
SpO2 - saturation, blood oxygen saturation,
measured by pulse oximetry
CO2 - partial pressure of carbon dioxide
СРАР (continuous positive airway pressure) - constant
positive airway pressure
1.1. Definition
Congenital pneumonia - acute infection with a predominant lesion of the respiratory sections of the lungs and the accumulation of inflammatory exudate inside the alveoli, detected during an objective and x-ray examination, as a rule, in the first 72 hours of life.
1.2. Etiology and pathogenesis
The cause of congenital pneumonia is intrauterine or intranatal infection of the fetus with microorganisms of various etiologies, transplacental, reproductive
walking or contact. Causative agents of congenital pneumonia:
bacteria Escherichia coli, Enterobacter aerogenes, Klebsiella spp., Pseudomonas aeruginosa, Group B Streptococcus, Staphylococcus epidermidis, Staphylococcus aureus, Haemophilus influenza, Klebsiella pneumoniae, Pneumococcus;
atypical pathogens: Chlamydia trachomatis, Urea-plasma aurealyticum, Mycoplasma hominis, Mycoplasma pneumoniae, Listeria monocytogenes, Treponema pallidum, Mycobacterium tuberculosis;
viruses: Herpes simplex virus, Cytommegalovirus (CMV), Respiratory syncytial virus, Rubella; mushrooms: Candida spp.
Pathogenesis and pathological anatomy
An important role in the development of congenital pneumonia is played by infectious and inflammatory diseases of the urinary and reproductive systems of the mother (pyelonephritis, chorioamnionitis, endometritis, etc.); gestational maturity of the fetus, the state of the surfactant system and the bronchopulmonary apparatus, malformations of the bronchial tree, intrauterine hypoxia, birth asphyxia, aspiration of meconium and amniotic fluid. Prematurity, respiratory distress syndrome (RDS), impaired cardiopulmonary adaptation, fetal hypoxia contribute to the development infectious process due to functional, morphological and immunological immaturity of lung tissue.
The disease develops as a result of hematogenous introduction of the pathogen in the last days or weeks of pregnancy or as a result of infection of the lungs when amniotic fluid enters them (infected with endometritis, chorioamnionitis, etc.) or when infected contents of the birth canal are aspirated. In all cases, bilateral lung damage is found (both alveoli and interstitium). These changes cause the occurrence of hypercapnia, hypoxemia, mixed acidosis and hypoxia after birth, deterioration of surfactant synthesis, which causes the appearance of atelectasis, parenchymal pulmonary edema, and increased intrapulmonary pressure. As a result of progressive hypoxia, acidosis and microcirculation disorders, multiple organ failure develops very quickly (first cardiopulmonary, then other organs).
The radiographic picture of pneumonia is determined by the type of tissue infiltration and the stage of inflammation.
Types of infiltration:
■ alveolar type of infiltration is observed when air-containing alveoli are filled with inflammatory exudate (seal, consolidation of air-containing spaces);
■ interstitial type of infiltration - observed when exudate fills the interalveolar spaces, while the alveoli contain air (ground glass symptom).
Stages of inflammation
I. Stage of infiltration (1st week of illness). Shading of the lung tissue without clear contours and boundaries, which, as a rule, is localized in the peripheral parts of the segments and lobes. In certain areas, shading may be limited to intersegmental or interlobar septa; in adjacent segments, interstitium reactions are detected.
II. Stage of resorption (2nd week of illness). The duration and intensity of infiltration decrease, visualization of lobular shading and focal shadows of various sizes is possible in combination with areas of lung tissue with normal or increased pneumatization against the background of increased lung pattern due to the interstitial component.
III. Stage of interstitial changes (end of the 2nd - beginning of the 3rd week). There are no infiltrative changes
interstitial changes at the site of infiltration in the form of peribronchial changes, mesh deformation of the lung pattern, heaviness are detected and detected.
1.3. Epidemiology
The incidence of pneumonia among full-term newborns, according to literary sources, is about 1%, premature - about 10%. Mortality in congenital pneumonia is 5-10%.
According to official statistics, in Russian Federation in 2015, congenital pneumonia was diagnosed in 0.98% of premature newborns with a birth weight of 1000 g or more and in 20.77% of newborns from 500 to 999 g. Mortality from congenital pneumonia in full-term newborns was 1.66%; born with a body weight of 1000 g or more - 2.3%, children born with extremely low body weight - 11.8% (form No. 32).
1.4. ICD 10 codes Congenital pneumonia (P23): P23.0 Viral congenital pneumonia
F23.1 Congenital pneumonia due to chlamydia F23.2 Congenital pneumonia due to staphylococci
P23.3 Congenital pneumonia due to group B streptococci
P23.4 Congenital pneumonia due to Escherichia coli
P23.5 Congenital pneumonia due to Pseudomonas P23.6 Congenital pneumonia due to other bacterial agents: Haemophilus influenzae, Klebsiella, Mycoplasma, streptococcus, excluding group B
P23.8 Congenital pneumonia due to other pathogens
P23.9 Congenital pneumonia, unspecified Less commonly, congenital pneumonia is caused by rubella, herpes simplex type II viruses, cytomegalovirus (CMV), and the disease can also be a manifestation of congenital bacterial sepsis, congenital tuberculosis, toxoplasmosis, listeriosis, malaria and candidiasis, then it is recorded under the code relevant infections (P35 - see section "Congenital infections"). Pneumonia as a symptom of early congenital syphilis is recorded under the code A50.
The term "neonatal pneumonia" is more capacious and combines congenital (P23), aspiration (P24) and acquired, including nosocomial, pneumonia. The latter, in accordance with ICD-10, are classified according to the etiological principle; for their statistical accounting, codes with the letter “J” are used (class X “Respiratory diseases”).
Neonatal pneumonias are classified (Table 1) as follows:
■ by the time of occurrence: intrauterine (congenital, which manifested itself in the first 72 hours of life) and neonatal (early and late);
Table 1. Classification of neonatal pneumonia (Sotnikova K.A., 1985)
Period of occurrence Etiology Type Severity Course
Intrauterine Viral. Bronchopneumonia: Mild. Acute.
(congenital). Microbial. - small focal; Medium-Subacute.
(acquired): Mycoplasma. - drain; Heavy - continuous;
Early, fungal. - mono- - with exacerbations and relapses.
Late Mixed and polysegmental; - interstitial No complications. With complications (otitis media, pneumothorax, pleurisy, etc.)
■ according to the prevalence of the process: focal, segmental, lobar, unilateral, bilateral;
■ according to the severity of the process: light, moderate, severe;
■ downstream: acute, subacute, protracted.
1.6. Clinical picture
Early clinical symptoms of congenital pneumonia are not specific:
■ respiratory disorders (tachypnea of 60 or more at rest, retraction of the intercostal space and / or retraction of the sternum, inspiratory retraction of the jugular notch above the sternum, swelling of the wings of the nose, foamy discharge from the mouth). These clinical signs are nonspecific and can be observed in other pathological conditions, in particular in critical birth defects heart (CHP). With the aim of differential diagnosis and exclusion of CHD, it is necessary to conduct a hyperoxic test, measurement of blood pressure on the lower and upper limbs, echocardiography (EchoCG), determine pre- and postductal blood oxygen saturation;
■ general signs of the disease and signs of infectious toxicosis: lethargy, muscular hypotonia/dystonia, "marbling" and gray coloration of the skin, pallor of the skin with perioral cyanosis and/or acrocyanosis, which is aggravated by excitement or by feeding, decreased tissue turgor, decreased or lack of a sucking reflex, refusal to feed, violation of thermoregulation (both hyperthermia and the inability to retain heat), the appearance of early jaundice (without the risk of developing hemolytic disease of the newborn (THN) according to AB0 and Rh factor);
■ physical signs:
on auscultation of the lungs - weakened or hard breathing, localized moist finely bubbling and crepitant rales, bronchial breathing can be heard when the foci merge. With weakened breathing, wheezing may not be heard;
with percussion of the chest - dullness of percussion sound over the projection of infiltration of the lung tissue.
All described clinical manifestations are nonspecific and can be observed in newborns against the background of other diseases.
left respiratory system Therefore, risk factors for the infectious process, X-ray and laboratory examinations are of great importance in the diagnosis.
2. Diagnostics
2.1. Anamnesis
The presence of risk factors on the part of the mother and child:
■ availability acute infection in the mother or exacerbation of chronic;
■ colonization of the mother's birth tract with group B streptococcus (GBS);
■ premature birth (<37 нед гестации);
■ prenatal rupture of amniotic fluid (anhydrous interval> 18 hours);
■ maternal temperature during labor >38°C;
■ maternal bacteriuria during this pregnancy;
■ chorioamnionitis;
■ violation of the cardiotocogram (CTG) of the fetus;
■ premature baby, low birth weight;
■ invasive procedures during pregnancy;
■ inadequate antibiotic therapy (ABT);
■ surgical treatment of the fetus and newborn;
■ non-compliance with infection control measures in maternity and neonatal wards.
2.2. Physical examination
On examination, an unstable temperature (>38.5 or<36 °С); снижение насыщения крови кислородом; тахипноэ >60/min or episodes of apnea; expiratory moan; retraction of pliable parts of the chest; weakened breathing, the presence of various rales in the lungs, lethargy, pallor, "marbling" and a grayish tint of skin color, refusal to suck; drowsiness or changes in neurological status; bloating; indigestion of food; tachycardia>180 per minute, deafness of heart sounds; decrease in the effectiveness of ongoing respiratory therapy, leading, among other things, to an increase in the parameters of artificial lung ventilation (ALV); possibly purulent contents in the trachea.
2.3. Instrumental examination
Comments. The radiological picture depends
on the phase and severity of the disease. A diffuse decrease in the transparency of the lung fields, a reticulogranular pattern and stripes of enlightenment in the region of the lung root (air bronchogram) are nonspecific and can be detected not only in congenital pneumonia, but also in early neonatal sepsis, RDS.
■ Bacteriological cultures (the contents of the pharynx, aspirate from the trachea, feces, if possible, blood, etc.) with the determination of the sensitivity of the isolated flora to antibiotics.
Comments. Determining the level of CRP and conducting a clinical blood test should be repeated after 48 hours, if it is difficult to make a diagnosis on the first day of a child's life. RDS is characterized by negative markers of inflammation and a negative result of a microbiological blood test. Increasing the level of CRP* is early sign bacterial infection in full-term children, while a similar pattern between its concentration in the blood of premature children and the presence of an infectious pathology in them has not been clearly proven.
■ General clinical analysis of blood.
■ It is recommended to conduct real-time PCR of blood for gram+, gramflora, TNV infections, viruses, atypical pathogens and fungi in case of prolonged stay of the mother in hospital during this pregnancy, repeated courses of antibacterial, hormonal and / or cytotoxic therapy, the presence of in the mother of implanted organs or devices (artificial valves), as well as in the case of risk factors for infection in the mother.
Comments. Carrying out PCR of blood depends on the technical capabilities of the laboratory.
Comments. The determination of blood lactate depends on the availability and technical capabilities of the express laboratory.
Comments. A meta-analysis of 22 randomized trials found that PCT is more sensitive in diagnosing nosocomial infection than congenital infection. Enhanced level PCT in blood serum on the 7th day of ABT indicates the need to continue or change antibiotic therapy. The determination of PCT is not a mandatory test in newborns, its implementation depends on the capabilities of the laboratory of the medical institution.
2.5. Criteria for the diagnosis of congenital pneumonia
To confirm the diagnosis, 2 groups of criteria are used: the main and auxiliary ones. The diagnosis of congenital pneumonia can be confirmed if the main and / or 3 (or more) auxiliary diagnostic signs are detected.
The main criterion for the diagnosis of congenital pneumonia
■ The presence of infiltrative shadows on the radiograph of the lungs (in the first 3 days of life).
Comments. X-ray symptoms of congenital pneumonia do not have the necessary specificity and are quite variable, so it is practically impossible to draw a conclusion about the etiological factor of the inflammatory process only on their basis. In most cases, there is a bilateral lesion of the lung tissue, as a rule, in the form of a patchy picture of the lungs - a combination of areas of compaction of the lung tissue and a compensatory increase in airiness. An effusion may be found in pleural cavities. Lung tissue changes associated with pleural effusion suggest bacterial pneumonia more likely than any other cause of respiratory distress, especially if group B streptococcus is the etiological factor.
Foci of compaction of the lung tissue, as a rule, affect several lobes. Pronounced compaction, limited to one single lobe, is relatively rare in newborns.
Auxiliary diagnostic criteria for congenital pneumonia
In table. 2 reflects the general signs for diagnosing sepsis and pneumonia in newborns and is used as
* The upper limit of the standard values for CRP is determined by the method used and the type of analyzer. NEONATOLOGY: news, opinions, training №4 2017
Table 2. Clinical and laboratory signs of the course of the infectious process in children with a post-conceptual age of less than 44 weeks
Clinical signs of infection
Changed body temperature
Body temperature less than 36°C or more than 38.5°C (hyperthermia) AND/OR
body temperature instability
Manifestations cardiovascular insufficiency
Bradycardia (mean heart rate less than the 10th percentile for age in the absence of β-blocker therapy or evidence for CHD)
Tachycardia (average heart rate over 180 per minute in the absence of external stimuli, prolonged drug and pain stimuli);
Other rhythm disturbances;
Arterial hypotension (average arterial pressure less than the 5th percentile for gestational age);
"marbling" of the skin;
Centralization of blood circulation with impaired perfusion of the skin (symptom " white spot» more than 3 s)
Respiratory disorders
Apnea episodes
Episodes of tachypnea
Increasing need for oxygen
Need for respiratory support
Manifestations of kidney failure
Decrease in diuresis less than 0.5 ml/kg per hour on the 1st day of life, less than 1 ml/kg per hour over the age of 1 day of life
Skin and subcutaneous tissue changes
Grayish color of the skin;
Sclerema
Manifestations from the side gastrointestinal tract
Lack of absorption of nutrition; bloating;
Weakening or absence of peristalsis on auscultation
Neurological manifestations
lethargy;
Hypotension;
Hyperesthesia;
Irritability;
convulsive syndrome
Manifestations hemorrhagic syndrome
petechial rash; stomach bleeding; pulmonary bleeding; macrohematuria; bleeding from injection sites
Other manifestations The presence of fluid in the pleural cavities from the 1st day of life; early onset jaundice;
hepatomegaly (in children> 1500 g at birth - more than 2.5 cm in the midclavicular line and more than 2 cm in children<1500 г), спленомегалия (в отсутствие признаков гемолитической болезни новорожденных); наличие других гнойно-воспалительных очагов у ребенка в первые 3 сут жизни
Leucopenia less than 5*109/l OR
Leukocytosis on the 1st-2nd day of life more than 30*109/l; on the 3rd-7th day of life more than 20 * 109 / l
The end of the table. 2
Laboratory signs of an infectious process
Absolute neutrophil count
Neutrophilia more than 20*109/l on the 1st-2nd day of life; more than 7*109/l after 3 days of life;
Neutropenia
Age, h Neutropenia with body weight >1500 g, cells/μL Age, h Neutropenia with body weight<1500 г, кл/мкл
0-6 <2000 0-6 <500
>6-12 <4000 >6-12 <1500
>12-24 <6000 >12-30 <1800
>24-48 <4000 >30-48 <1500
>48-72 <2000 >48 <1100
The ratio of the proportion of young forms to the total number of neutrophils (neutrophil index)
More than 0.2.
Features of the morphology of neutrophils (examined in doubtful cases)
Toxic grit;
Vacuolization;
Appearance of Loli bodies (basophilic areas in the cytoplasm)
Thrombocytopenia
Less than 1.5x1011/l
Increased levels of inflammatory markers
Elevated levels of C-reactive protein in the blood (the upper limit of the normative values of CRP is determined by the method used and the type of analyzer).
metabolic acidosis
Serum lactate over 2 mmol/l
Placenta examination
Changes in the placenta, such as deceduitis, funizitis, tissue infiltration, may indirectly indicate the implementation of the infectious process in the newborn and are an additional factor in the diagnosis of pneumonia (depending on the level of the medical institution providing care for newborns)
Chest radiograph
Strengthening of the bronchovascular pattern;
Pattern enhancement due to mesh/grain structures, especially on radiographs in case of combination with surfactant deficiency AND/OR
Local decrease in the transparency of the lung tissue with increased airiness of the parts of the lung tissue involved in the process of respiration
Episodes of glucose intolerance recorded at least twice (at an age-appropriate rate of glucose intake)
■ Hypoglycemia less than 2.6 mmol/l;
■ hyperglycemia more than 10 mmol/l
Inflammatory changes in the clinical analysis of urine Leukocyturia over 10-15 per field of view in combination with bacteriuria and proteinuria (protein content over 0.2 mg / l) - after 48 hours
improved auxiliary diagnostic criteria for congenital pneumonia. The presence of at least two clinical and one laboratory sign indicates the course of an infectious process in a child.
2.6. Differential Diagnosis
■ Transient tachypnea of newborns;
■ early neonatal sepsis;
■ meconium aspiration syndrome;
■ other types of aspiration (amniotic fluid, blood, milk);
■ air leakage syndrome;
■ persistent pulmonary hypertension in newborns;
■ congenital malformations of the lungs (cystic adenomatosis, aplasia, pulmonary hypoplasia, etc.);
■ congenital diaphragmatic hernia;
■ congenital heart disease;
■ other reasons for the development of respiratory disorders of extrapulmonary origin.
3. Treatment of congenital pneumonia
3.1. Conservative treatment
Treatment of congenital pneumonia should include measures aimed simultaneously at several directions.
■ Etiotropic therapy - the impact directly on the infectious agent - the causative agent of the disease.
■ Pathogenetic therapy - correction of changes in homeostasis and manifestations of multiple organ failure.
■ Symptomatic therapy.
3.2. Etiotropic therapy
Antibacterial therapy (ABT) is the main element of therapy for congenital pneumonia.
■ Antibiotic therapy for suspected congenital pneumonia is indicated as early as possible after birth for the following categories of children with respiratory disorders: very low birth weight (VLBW), extremely low birth weight (ELBW), and those requiring conducting IVL. It is preferable to start ABT no later than 2 hours of life, for newborns with ENMT - in the delivery room. The first introduction of drugs of the starting scheme is carried out simultaneously.
■ ABT in the presence of indications based on the results of the primary clinical and laboratory examination. This category includes patients over 1500 g at birth who had respiratory problems, but did not require conventional ventilation, as well as those who are on non-invasive respiratory therapy [CPAP spontaneous breathing (CPAP), non-invasive ventilation] or patients without respiratory therapy.
■ ABT, started on suspicion on the first day of life, is canceled in the absence of clinical, laboratory and instrumental data confirming the course of congenital pneumonia within 72 hours of life.
■ When a diagnosis of pneumonia is established, the empirical ABT regimen continues for 7 days (the minimum course of ABT for congenital pneumonia), then a clinical and laboratory examination is carried out with the control of inflammation markers.
When the levels of inflammation markers and clinical blood test (CBC) normalize, ABT is canceled.
Starting ABT schemes [Appendix D] .
■ Scheme A: the use of empirical ABT - a combination of drugs ampicillin + gentamicin.
■ Scheme B: provides for antibiotic therapy for newborns whose mothers have confirmed seeding of flora resistant to the drugs of the empirical ABT regimen. It is advisable to use protected penicillins.
■ Comments. Preference is given to parenteral administration of antibiotics (intravenous administration). It is not recommended to prescribe drugs containing amoxicillin and clavulanic acid due to the possible adverse effects of acid on the intestinal wall, especially in preterm infants. It is not advisable to include cephalosporins in the starting regimen of antibiotic therapy instead of semi-synthetic penicillin due to the lack of activity against Listeria monocitogene.
ratam. In the absence of sensitivity of the isolated pathogens to the drugs of the starting regimen, it is necessary to switch to antimicrobial drugs to which sensitivity has been detected.
The duration and tactics of antibiotic therapy are determined in each case individually and depend on the severity of the child's condition and the normalization of clinical and laboratory data.
3.3. Pathogenetically substantiated intensive care
Due to the fact that immaturity and prematurity contribute to the development of pneumonia, clinical manifestations in the first hours and days of life are nonspecific, the directions of therapy are practically no different from those for RDS in newborns and the principles of its application are the same [see. Clinical guidelines "Respiratory distress syndrome", 2017].
Comments. See the Methodological letter of the Ministry of Health of Russia "Primary and resuscitation care for newborn children" dated 04/21/2010 No. 15-4 / 10 / 2-320.
Comments. Clamping and cutting the umbilical cord 60 s after birth in preterm infants with VLBW and ELBW lead to a significant reduction in the incidence of necrotizing enterocolitis, intragastric bleeding (IVH0, sepsis, and a decrease in the need for blood transfusions.
Comments. Respiratory therapy is a key focus in the treatment of respiratory disorders in newborns, including children with congenital pneumonia. It should solve the following tasks: achieving and maintaining adequate gas exchange and alveolar ventilation, minimizing the risk of ventilator-associated lung injury and impaired cardiohemodynamics, achieving patient comfort by eliminating desynchronization. To date, a number of new methods of respiratory therapy for newborns have appeared, including in the delivery room. In mechanical ventilation, volume-controlled ventilation is preferred because this strategy determines adequate and constant tidal volume, as well as minute ventilation at low airway pressure. Early initiation of respiratory therapy allows to reduce its duration, limiting itself to softer ventilation parameters.
With the ineffectiveness of CPAP and mechanical ventilation with a mask.
Comments. Mechanical ventilation in preterm infants is carried out with bradycardia persisting against the background of CPAP and / or with prolonged
(more than 5 min) lack of spontaneous breathing. Invasive ventilation in the delivery room under tidal volume control in very preterm patients is a promising technology to minimize ventilator-associated lung damage.
In the delivery room when providing primary and resuscitation care to newborns.
Comments. See the Methodological letter of the Ministry of Health of Russia "Primary and resuscitation care for newborn children" dated 04/21/2010 No. 15-4 / 10 / 2-3204.
Premature babies with respiratory problems
indications regardless of birth weight.
Comments. See Methodological letter of the Ministry of Health of Russia "Primary and resuscitation care for newborn children" dated 04.21.2010 No. 15-4 / 10 / 2-3204 and Clinical recommendations "Respiratory distress syndrome", 2017.
Surfactant can be used in preterm infants with RDS complicated by congenital pneumonia, but a higher dosage or frequency of administration is required.
Comments. See Methodological letter of the Ministry of Health of Russia "Primary and resuscitation care for newborns" dated April 21, 2010 No. 15-4 / 10 / 2-3204 and Clinical recommendations. Respiratory Distress Syndrome, 2017.
Comments. Indications for mechanical ventilation are also severe concomitant conditions: shock, convulsive status, pulmonary hemorrhage. It is necessary to minimize the duration of invasive mechanical ventilation. If possible, mechanical ventilation with tidal volume control should be performed, which reduces its duration and reduces the incidence of complications such as bronchopulmonary dysplasia and IVH. A prerequisite for the successful use of this type of respiratory therapy in newborns is the ability to regularly monitor the gas composition of the blood. Routine sedation and analgesia is not recommended for all ventilated children.
The inefficiency of traditional mechanical ventilation is an indication for switching to high-frequency oscillatory lung ventilation (HFOV). With HFOV, due to the stabilization of the volume of the alveoli, there is a decrease in atelectasis, an increase in the area of gas exchange and an improvement in pulmonary blood flow. As a result of properly conducted therapy,
an adequate ventilation-perfusion ratio is established, which leads to an improvement in gas exchange in the lungs.
Basic principles of infusion therapy:
■ calculation of fluid volume and parenteral nutrition based on physiological needs and pathological losses;
■ the infusion program is compiled taking into account the individual characteristics of the postnatal maturation of kidney function;
■ the need for clinical and laboratory monitoring of water and electrolyte balance to assess the adequacy of the infusion program;
■ in case of violation of peripheral and / or central hemodynamics, the appointment of cardiotonic drugs is indicated.
3.4. Symptomatic therapy
Symptomatic therapy involves the creation of optimal conditions for nursing newborns.
■ Depending on the severity of the condition, a newborn with suspected congenital pneumonia should be transferred to a neonatal intensive care unit, intensive care unit (ICU), or neonatal pathology unit.
■ The child is shown staying in the microclimate of the incubator, limiting sensory stimulation (protection from light, noise, touch), controlling body temperature depending on thermoregulation, postural support, and preventing pain.
■ Antihemorrhagic therapy is used for hemorrhagic disorders.
■ Start enteral nutrition as early as possible, breast milk is preferred.
4. Rehabilitation
In full-term children who have had congenital pneumonia, the long-term prognosis is usually favorable. In very premature babies, there is a risk of developing bronchopulmonary dysplasia. The development of a nosocomial infection in the NICU worsens the outcome and prognosis of the underlying disease.
5. Prevention and follow-up
Prevention of congenital pneumonia is the timely detection and treatment of infectious diseases in the mother during pregnancy.
The strictest observance of the sanitary and epidemiological regime in the maternity hospital, departments for newborns and premature babies is necessary.
A young child who has had pneumonia is monitored for 1 year. It is necessary for the maximum stay of the child in the fresh air, good nutrition, physiotherapy exercises (LFK), massage, tempering procedures.
Criteria for assessing the quality of medical care
Group name: congenital pneumonia.
ICD-10 code: P23.
Type of medical care: specialized, including high-tech.
Age group: children.
Conditions for the provision of medical care: inpatient.
Form of medical care: emergency.
Quality criterion Performance evaluation
The degree of severity of respiratory disorders was assessed on the scales Yes / No
Performed pulse oximetry with monitoring of heart rate from the moment of detection Yes / No
respiratory disorders (if present in the delivery room)
Air/oxygen supplementation provided and/or non-invasive mechanical ventilation Yes/No
lungs, and/or conventional mechanical ventilation, and/or HFOV (depending on medical indications)
Vital signs were monitored (respiratory rate, saturation level Yes/No
hemoglobin with oxygen, heart rate, blood pressure, diuresis)
The study of the acid-base state and blood gases (pH, PaCO2, Pa02, BE, Yes / No) was performed
lactate - if possible) in the detection of respiratory disorders
Completed general (clinical) blood test (CBC), CRP and microbiological blood tests Yes/No
(if technically possible) no later than 24 hours from the moment of detection of respiratory disorders
Performed repeated studies of the CBC, CRP after 48 hours, in case of negative results Yes / No
in the first days of life
A chest X-ray was performed no later than 24 hours from the moment of detection Yes / No
respiratory disorders
Empiric antibiotic therapy was prescribed within 1 hour from the moment of receipt Yes/No
results of UAC, SRP
Annex A1. Methodology for the development of clinical guidelines
■ pediatrics;
■ neonatology;
■ obstetrics and gynecology.
Methodology
Methods used to collect/select evidence: electronic database searches.
Description of the methods used to collect/select evidence: the evidence base for recommendations are publications included in the Cochrane Library, the EMBASE and MEDLINE databases, and the electronic library (www.eLibrary.ru). The search depth was 5 years.
Methods used to assess the quality and strength of evidence:
■ expert consensus;
Methods used to analyze the evidence:
■ Systematic reviews with tables of evidence.
Description of the methods used to analyze the evidence
When selecting publications as potential sources of evidence, the methodology used in each study is reviewed to ensure its validity. The outcome of the study affects the level of evidence assigned to the publication, which in turn affects the strength of the recommendations that follow from it.
The methodological study is based on several key questions that focus on those features of the study design that have a significant impact on the validity of the results and conclusions. These key questions may vary depending on the types of studies and the questionnaires used to standardize the publication evaluation process.
The evaluation process, of course, can be affected by the subjective factor. To minimize potential errors, each study was evaluated independently, ie. at least 2 independent members of the working group. Any differences in assessments were already discussed by the entire group. If it was impossible to reach a consensus, an independent expert was involved.
Evidence tables were filled in by members of the working group.
Methods used to formulate recommendations: expert consensus.
■ external expert evaluation;
■ internal peer review.
These draft recommendations have been peer-reviewed by independent experts who were asked to comment primarily on the extent to which the interpretation of the evidence underlying the recommendations is understandable. Comments were received from primary care physicians and district therapists regarding the intelligibility of the presentation of recommendations and their assessment of the importance of recommendations as a working tool in everyday practice.
The draft was also sent to a non-medical reviewer for comments from a patient perspective.
AT community-acquired pneumonia (CAP) is an acute infectious inflammation of the alveoli that occurs outside the hospital and manifests itself with clinical and (or) radiological signs that are not associated with other causes
Dominant causative agents of EP - Streptococcus pneumoniae haemophilus influenzae Mycoplasma pneumoniae Chlamydia pneumoniae Legionella pneumophila Staphylococcus aureus
Anaerobes.
VP classification
- Pneumonia in patients without comorbidities
- Pneumonia against the background of severe somatic diseases
- aspiration pneumonia.
Clinical symptoms of pneumonia Respiratory symptoms (cough, shortness of breath, chest pain, crepitus, bronchial breathing, dullness on percussion),
Symptoms of intoxication (fever, chills, headache, cerebral symptoms, etc.),
Decompensation of concomitant pathology (COPD, heart failure, diabetes mellitus, etc.).
Additional diagnostic features Laboratory (neutrophilic leukocytosis or leukopenia),
X-ray (pulmonary infiltrate, pleural effusion),
Bacterioscopy of sputum with Gram stain,
Serological diagnostics (antibodies to mycoplasma and chlamydia).
Gram-staining of sputum is an important guideline for choosing the initial antibiotic, taking into account the "gram-belonging" of microorganisms. Especially appropriate should be considered bacterioscopy and culture of sputum containing a sufficient number of neutrophils in a hospital setting. A negative Gram-stained sputum does not always indicate the absence of microorganisms in the sputum and may be due to their insufficient number (less than 104). If about 10 microorganisms are found in one field of view, this means that their number is at least 10 5 and approaches the diagnostic titer.
Serological diagnosis may be of value in the verification of atypical microorganisms (usually retrospective) based on the level of IgG and IgM antibodies after 2-3 weeks.
The wording of the diagnosis of pneumonia should reflect:
Nosological form (community-acquired or nosocomial),
The etiological variant of EP (indicative or verified),
Background pathology (character, activity),
Localization and prevalence of pulmonary inflammation (according to X-ray examination),
Presence of complications (pulmonary and extrapulmonary),
severity of pneumonia
The phase of the disease (peak, resolution),
Current (usual, protracted).
Making key decisions in the management of a patient with CAP Determination of the place of treatment (outpatient or inpatient),
The choice of the initial antibacterial drug (AP),
Evaluation of the effectiveness of AP after 48-72 hours and making a decision on further treatment tactics,
Duration of antibiotic therapy (AT),
Making a decision to switch from parenteral to oral administration of AP,
Necessity and indications for symptomatic therapy.
In mild cases, treatment can be done on an outpatient basis. Indications for hospitalization are:
Age over 65 years old,
The presence of severe comorbidity (COPD, heart failure, diabetes mellitus, immunodeficiency states, etc.),
Impossibility of adequate care and fulfillment of medical prescriptions at home,
The preference for inpatient treatment for patients or their family members,
The presence of one of the criteria for a severe course of pneumonia,
Failure of antibiotic therapy within 72 hours.
Antibacterial drugs prescribed for community-acquired pneumonia Aminopenicillins (amoxicillin),
Protected penicillins (amoxicillin/clavulanic acid, ampicillin/sulbactam),
Macrolides (erythromycin, clarithromycin, spiramycin, midecamycin, etc.),
Cephalosporins I-III generations,
Fluoroquinolones (ciprofloxacin, moxifloxacin),
Lincosamines (clindamycin, lincomycin).
Requirements for AP prescribed for the treatment of pneumonia Activity against the main causative agents of pneumonia,
Optimal concentration in lung tissue and alveolar macrophages,
Good bioavailability of AP when administered orally,
No clinically significant interactions with other drugs
long half-life,
Minimal resistance of microorganisms,
Relatively low toxicity and safety,
The presence of the drug in various dosage forms.
Duration of AT The duration of the AT of community-acquired pneumonia is determined by various factors, including the response to therapy, the severity of pneumonia, the presence of complications, the nature of the pathogen (etiological variant). In cases of uncomplicated pneumonia caused by S. pneumoniae, H. Influenzae, the duration of AT should not exceed, as a rule, 7-10 days. With pneumonia caused by intracellular pathogens (Legionella, Mycoplasma), as well as in patients with complications (abscess), the duration of treatment can be up to 21 days. X-ray resolution of pneumonia, normalization of ESR occur at a later date than the disappearance of signs of intoxication and respiratory symptoms.
In order to ensure greater comfort of treatment and reduce the cost of treatment, upon the onset of a clinical effect within 48-72 hours, it is possible to switch from parenteral to oral administration of AP. Requirements for switching from parenteral to oral route of antibiotic administration:
The presence of an antibiotic in oral and parenteral form,
The effect of a parenterally administered antibiotic,
The stable condition of the patient
The possibility of taking drugs inside,
Absence of intestinal pathology,
High bioavailability of oral antibiotic.
Special situations in the treatment of patients with pneumonia Pregnancy,
The presence of concomitant pathology (liver, kidneys, etc.),
Hypersensitivity to various antibacterial drugs,
Pneumonia caused by the so-called. atypical pathogens,
Complicated pneumonia,
Severe pneumonia with an unknown pathogen,
Pneumonia of a prolonged course,
Lack of effect from the initial AP.
When choosing AP for the treatment of pneumonia in pregnant women, the appointment of fluoroquinolones, clindamycin, metronidazole is erroneous. In addition, aminoglycosides, vancomycin, imipenem should be prescribed with caution.
The presence of concomitant pathology with functional disorders of the kidneys and liver creates difficulties in conducting AT, which can lead to errors in the choice of AP, its dosage, routes of administration, duration of AT, etc. At the same time, it is erroneous to prescribe potentially nephrotoxic APs (aminoglycosides, carbapenems) without dose adjustment in patients with concomitant renal failure. It is also dangerous in such situations to combine AP with nephrotoxic properties (aminoglycosides and cephalosporins, with the exception of cefoperazone). If the patient has renal insufficiency, preference should be given to the choice of AP with predominantly extrarenal excretion of the drug in the bile or by metabolism in the liver (cefoperazone, macrolides, clindamycin, pefloxacin). Especially it is necessary to take into account the presence of concomitant, often multiple pathology with functional disorders of organs and systems in elderly and senile patients. Age-related decrease in glomerular filtration rates, along with a high incidence of nephroangiosclerosis in the elderly, should be one of the factors influencing the choice of AP. The presence of pathology from the gastrointestinal tract (in particular, intestinal absorption disorders) limits the possibility of prescribing AP orally and performing stepwise therapy. Additional difficulties in choosing AP and assessing the risk of adverse side effects may occur in patients receiving various drugs (theophyllines, cardiac glycosides, loop diuretics, calcium salts, etc.) for concomitant pathology. In such situations, APs with minimal drug interactions should be preferred.
In the presence of reliably established hypersensitivity to penicillin, other b-lactam APs (cephalosporins, carbopenems) should not be prescribed. Alternative AP can be fluoroquinolones, macrolides. However, reactions of a different origin (vascular, vegetative, etc.) can often be taken as "allergy to antibiotics", in connection with which it is necessary to critically evaluate the indications of patients for such "intolerance" and analyze the existing situation more carefully. At the same time, intradermal tests for AP are dangerous, since there is the same danger of severe anaphylactic reactions.
Pneumonia caused by L. pneumophilla, Mycoplasma pneumoniae, Chlamydia pneumoniae (the so-called atypical pneumonia), have a number of epidemiological and clinical features, which causes not only difficulties in diagnosis, but also AT of this etiological variant of pneumonia. Features of atypical pneumonia are the following:
The main causative agents - Mycoplasma, Chlamydia, Legionella,
Intracellular localization of pathogens,
Frequent extrapulmonary symptoms
special epidemiological situations,
Symptoms of ARVI at the onset of the disease ( Mycoplasma),
Failure to detect pathogens in sputum
Specific serological data,
Ineffectiveness of b-lactam antibiotics,
The effectiveness of macrolides, tetracyclines, fluoroquinolones.
severity of pneumonia. The main problems of severe community-acquired pneumonia:
Decompensation of concomitant pathology,
Difficulties AT,
Frequent treatment in intensive care units and intensive care units,
Worse prognosis compared to milder pneumonias
High mortality, especially among hospitalized patients,
High cost of treatment.
Basic principles of treatment of severe community-acquired pneumonia:
Verification of the severity of pneumonia,
Mandatory hospital treatment
The fastest onset of AT,
The appointment of an antibacterial drug (drugs) that maximally covers the likely pathogens of pneumonia,
Mandatory prescription of the drug (drugs) intravenously,
The feasibility of combined antibiotic therapy,
Careful monitoring of the patient's condition
Timely change of the drug (drugs) in the absence of effect,
Using step AT,
Adequate symptomatic and supportive therapy.
There are obvious difficulties in deciding on the choice of AP in patients with severe pneumonia, especially since the treatment of severe pneumonia should begin as early as possible. You should focus on the most common causative agents of severe pneumonia, which are considered S. pneumoniae, S. aureus, Enterobactericae, Legionella pneumophila. At the same time, pathogens such as Mycoplasma pneumoniae, H. influenzae usually do not lead to a severe course of the disease. In the conditions of empirical AT of severe pneumonia, the prescribed AP should cover all possible etiologically significant pathogens. If with community-acquired pneumonia of a mild course, monotherapy can be limited to the appointment of aminopenicillins (including protected ones) or macrolides, then in severe pneumonia, combined AT is justified. Almost all clinical recommendations for the treatment of severe pneumonia include third-generation cephalosporins (cefotaxime, ceftriaxone) in combination with parenteral macrolides (erythromycin, clarithromycin) or protected penicillins (amoxicillin/clavulanic acid) in combination with macrolides. The expediency of combining b-lactam antibiotics with macrolides in the treatment of severe pneumonia is due to the likelihood of legionella pneumonia and the difficulties of its etiological verification. When prescribing combined AT with third-generation cephalosporins in combination with macrolides, mortality in community-acquired pneumonia (especially among elderly patients) is lower compared with monotherapy with third-generation cephalosporins. To date, there are a number of studies indicating the clinical and bacteriological efficacy of respiratory fluoroquinolones (levofloxacin, moxifloxacin) as monotherapy in the treatment of severe pneumonia, comparable to the results of combined antibiotic therapy with cephalosporins or protected penicillins in combination with macrolides.
Protracted pneumonia with delayed resolution Factors that determine prolonged radiological resolution of pneumonia:
Age over 50,
The presence of concomitant pathology (COPD, diabetes mellitus, alcoholism, tumors, etc.),
severity of pneumonia
The nature of the pathogen (legionella, chlamydia).
Lack of effect from the initial AP. The generally accepted period for assessing the effectiveness of AP is 48-72 hours from the moment of its appointment. The criterion for the effectiveness of AP is usually a decrease or normalization of the patient's body temperature, a decrease in signs of intoxication. In cases where fever from the very beginning of the disease is not expressed or is absent at all, one has to focus on other signs of intoxication (headache, anorexia, cerebral symptoms, etc.), as well as on the absence of progression of the disease during the period of treatment. Continuation of AT, despite its inefficiency, delays the appointment of another, more adequate AP, contributes to the progression of pulmonary inflammation, the occurrence of complications, lengthens the treatment time, increases the risk of side (toxic) effects of AT and the development of antibiotic resistance.
In cases of ineffectiveness of the initial AP, it may be difficult to choose another antibiotic. In the absence of microbiological data, the principle of choosing an AP remains the same - i.e. orientation to the clinical situation, taking into account the ineffectiveness of the initial AP, which, to a certain extent, should be an additional guideline for choosing a second AP. Thus, the lack of effect from b-lactam APs (penicillins, cephalosporins) in a patient with community-acquired pneumonia suggests legionella or mycoplasmal pneumonia (taking into account, of course, other signs), which makes it reasonable to prescribe macrolides (erythromycin, spiramycin, clarithromycin, etc.) or fluoroquinolones (pefloxacin, levofloxacin).
The tactics of managing patients with a protracted course of pneumonia is shown in Figure 1.
Rice. 1. Tactics for prolonged radiological resolution of pneumonia
The main reasons for the ineffectiveness of the initial AP may be the following:
Misdiagnosis of pneumonia and the presence of another disease,
Inadequate initial AP,
Severe pneumonia,
Presence of undiagnosed complications
Inadequate dose, route of administration of AP.
One of the reasons for the ineffectiveness of the treatment of pneumonia may be inadequate doses of AP, which do not create the concentration in the blood necessary for the eradication of the corresponding pathogen. Errors in choosing the optimal dose can be associated with the appointment of both an insufficient single dose and an incorrect dosing regimen (insufficient frequency of administration). Given the presence of some AP so-called. post-antibiotic effect (the ability of the drug to inhibit the growth of microorganisms even with a decrease in the level of AP in the blood below the MIC), when prescribing such drugs (tetracyclines, fluoroquinolones, aminoglycosides), a sufficient single dose is important, and the intervals between injections may be longer. On the other hand, β-lactam APs (penicillins, cephalosporins of I and II generations), with the exception of carbapenems, are practically devoid of a post-antibiotic effect; more frequent (without gaps) administration of the drug.
Antibiotic resistance . Rational AT of pneumonia requires taking into account the degree of risk of antibiotic resistance of some microorganisms, for example, resistance S. pneumoniae to penicillin. Risk factors for penicillin resistance S. pneumoniae include: the age of patients less than 7 years and older than 60 years, the presence of severe somatic diseases, frequent and prolonged treatment with antibiotics, living in nursing homes. At high risk of penicillin resistance S. pneumoniae administration of macrolides may also be ineffective, since there may be cross-resistance to macrolides. At the same time, resistance S. pneumoniae to penicillin and macrolides does not correlate with resistance to respiratory fluoroquinolones, which makes it rational and reasonable to choose respiratory fluoroquinolones (levofloxacin, moxifloxacin) in such situations. Another problem of antibiotic resistance is the production H. influenzae b-lactamase, which is usually observed in COPD patients who often receive AP due to frequent exacerbations of the disease. With this in mind, with the development of pneumonia against the background of COPD, the appointment of protected penicillins (amoxicillin / clavulanate, ampicillin / sulbactam) is justified. The latter are ineffective against penicillin-resistant S. pneumoniae, since the mechanisms of resistance to penicillin in S. pneumoniae and H. influenzae are different (decrease in the affinity of penicillin-binding proteins). At the same time, "protected" penicillins can remain active against penicillin-resistant staphylococci that produce beta-lactamase. Therefore, in situations with a high probability of staphylococcal community-acquired pneumonia (after influenza, chronic alcohol intoxication), the appointment of inhibitor-protected penicillins is justified. It is irrational to prescribe co-trimoxazole or tetracycline as the initial AP for community-acquired pneumonia due to the high level of resistance to these APs of the main causative agents of pneumonia.
Situations not requiring continuation of AT or change of AP subfebrile temperature,
Persistence of dry cough,
Presence of crepitant wheezing
Preservation of infiltration with a clear positive dynamics according to X-ray examination,
An increase in ESR (with normalization of the number of leukocytes and blood counts).