Acute inflammatory diseases of the pharynx and larynx
Acute inflammation of the pharynx Acute inflammation of the nasopharynx To line. The main complaints of patients are discomfort in the nasopharynx - burning, tingling, dryness, often accumulation of mucous secretion; headache localized in the occipital region. Children often have difficulty breathing and nasal sound. With the predominant localization of the process in the region of the mouths auditory tubes there is pain in the ears, hearing loss by the type of sound conduction. In adults, this disease occurs without a sharp deterioration in the general condition, and in children the temperature reaction is significant, in particular, in cases where inflammation spreads to the larynx and trachea. Enlarged and painful cervical and occipital lymph nodes. Differential Diagnosis should be carried out with diphtheria nasopharyngitis (with diphtheria, dirty gray raids are usually visualized; examination of a smear from the nasopharynx usually allows you to clearly establish the nature of the diphtheria lesion); with a congenital syphilitic and gonococcal process (here other signs come to the fore - gonorrheal conjunctivitis, with lues - hepatosplenomegaly, characteristic skin changes); with diseases of the sphenoid sinus and cells of the ethmoid labyrinth (here, X-ray examination helps to establish the correct diagnosis). Treatment. Infusions are carried out in each half of the nose 2% (for children) and 5% (for adults) solution of protargol or collargol 3 times a day; with severe inflammation, a 0.25% solution of silver nitrate is poured into the nasal cavity, and then vasoconstrictor drops. Carrying out general anti-inflammatory and antibacterial treatment is justified only with a pronounced temperature reaction and the development of complications. The appointment of multivitamins, physiotherapy - quartz on the soles of the feet, UHF on the nose area is shown.
Acute inflammation of the oropharynx (pharyngitis) Clinic. In acute pharyngitis, most often patients complain of dryness, soreness and soreness in the throat. The pain may radiate to the ear when swallowing. With pharyngoscopy, hyperemia and swelling of the mucous membrane of the oropharynx, an increase and bright hyperemia of lymphoid granules located on the back of the pharynx are determined. Severe forms of acute pharyngitis are accompanied by an increase in regional lymph nodes, in children, in some cases, a temperature reaction. The process can spread both upwards (involving the nasopharynx, the mouths of the auditory tubes) and downwards (on the mucous membrane of the larynx and trachea). The transition to chronic forms is usually due to the ongoing exposure to a pathogenic factor (occupational hazard, chronic somatic pathology). Differential diagnosis in children, it is carried out with gonorrheal pharyngitis, syphilitic lesions. In adults, pharyngitis (in the case of its non-infectious genesis) should be considered as a manifestation of an exacerbation of chronic somatic pathology, primarily a disease of the gastrointestinal tract (since the pharynx is a kind of “mirror” that reflects problems in the organs located below). Treatment consists in the exclusion of irritating food, the use of inhalations and sprays of warm alkaline and antibacterial solutions, with a general reaction of the body, the appointment of paracetamol is indicated, as well as drinking plenty of liquids rich in vitamin C. With severe edema, the appointment of antihistamines is indicated.
Angina
Among clinicians, it is customary to subdivide all available forms of angina into vulgar (banal) and atypical ..
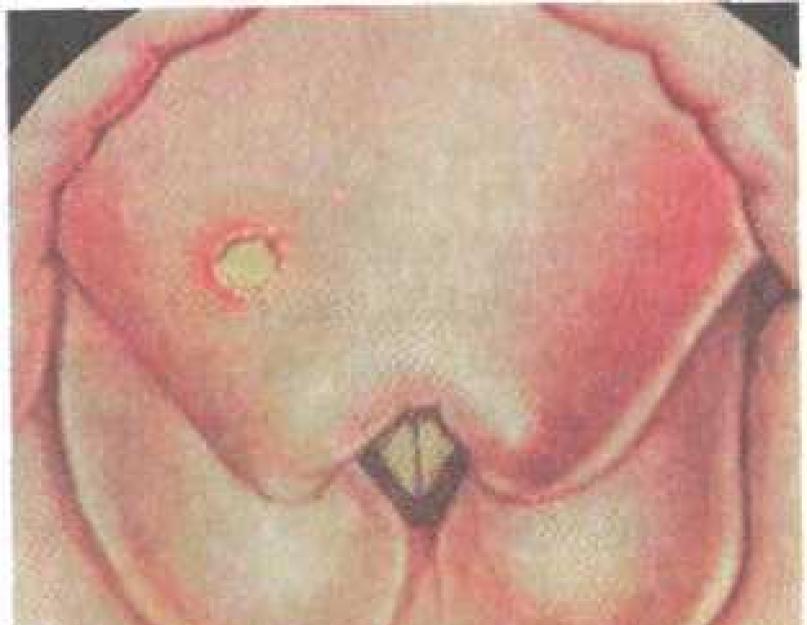
Vulgar (banal) tonsillitis Vulgar (banal) tonsillitis is mainly recognized by pharyngoscopy signs. For angina vulgaris, four common signs are characteristic: 1) severe symptoms of general intoxication of the body; 2) pathological changes in the palatine tonsils; 3) the duration of the process is not more than 7 days; 4) bacterial or viral infection as a primary factor in etiology. There are several forms: Catarrhal angina begins acutely, there is a burning sensation, perspiration, slight pain when swallowing. On examination, diffuse hyperemia of the tissue of the tonsils, the edges of the palatine arches is revealed, the tonsils are enlarged in size, sometimes covered with a film of mucopurulent exudate. Tongue dry, lined. Regional lymph nodes are moderately enlarged. Follicular angina usually begins acutely - with an increase in body temperature to 38-39 0 C, a sharp pain in the throat, aggravated by swallowing, general symptoms of intoxication are more pronounced - headache, sometimes back pain, fever, chills, general weakness. In the blood, pronounced inflammatory changes - neutrophilia up to 12-15 thousand, moderate stab shift to the left, eosinophilia, ESR reaches 30-40 mm / h. Regional lymph nodes are enlarged and painful. With pharyngoscopy - diffuse hyperemia and infiltration of the soft palate and arches, enlargement and hyperemia of the palatine tonsils, numerous festering follicles are determined on their surface, usually opening 2-3 days from the onset of the disease. Lacunar angina runs more difficult. When viewed on the hyperemic surface of the palatine tonsils, yellowish-white plaques are observed, easily removed with a spatula, bilateral localization. The phenomena of intoxication are more pronounced. Fibrinous (fibrinous-membranous) angina is a variation of the two previous sore throats and develops when bursting festering follicles or fibrinous deposits form a film. Here it is necessary to carry out differential diagnosis with diphtheritic lesions (based on bacteriological examination of the smear). Treatment. The basis of rational treatment of angina consists of compliance with a sparing regimen, local and general therapy. In the first days, bed rest is required, the allocation of individual dishes, care items; hospitalization in the infectious diseases department is necessary only in severe and diagnostically unclear cases of the disease. Food should be soft, non-irritating, nutritious, drinking plenty of water will help detoxify. When prescribing drugs, a comprehensive approach is required. The basis of treatment is antibiotic therapy (preference is given to antibiotics a wide range actions - semi-synthetic penicillins, macrolides, cephalosporins), a course of 5 days. The appointment of antihistamines will help stop the edema, which basically provokes pain. With severe intoxication, it is necessary to monitor the state of the cardiovascular and respiratory systems. In terms of local treatment, it is advisable to use drugs that have a local anti-inflammatory, analgesic and antiseptic effect (Septolete, Strepsils, Neo-Angin). Rinses with drugs that have a complex effect (OKI, texetidine) are also highly effective. Phlegmonous angina (intratonsillar abscess) is relatively rare, usually as a result of purulent fusion of the tonsil area; this lesion is usually unilateral. In this case, the tonsil is hyperemic, enlarged, its surface is tense, palpation is painful. Small intratonsillar abscesses usually open spontaneously and may be asymptomatic, but this mainly occurs when the abscess breaks into the oral cavity, when it is emptied into the paratonsillar tissue, a peritonsillar abscess clinic develops. Treatment consists of a wide opening of the abscess, with tonsillectomy indicated for recurrence. Herpangina develops mainly in young children, is highly contagious, and is usually spread by airborne droplets, less often by fecal-oral. Caused by adenoviruses, influenza virus, Coxsackie virus. The disease begins acutely, with fever up to 38-40 0 C, sore throat when swallowing, headache and muscle pain develops, vomiting and diarrhea are also not uncommon as signs of general intoxication. When pharyngoscopy - diffuse hyperemia in the soft palate, on the entire surface of the oropharyngeal mucosa there are small reddish vesicles that resolve after 3-4 days. For atypical angina applies primarily Simanovsky-Vincent's angina(the causative agent is a symbiosis of a fusiform bacillus and a spirochete of the oral cavity), the basis for making the correct diagnosis here is a microbiological examination of the smear. The differential diagnosis of such tonsillitis should be carried out with diphtheria of the pharynx, syphilis of all stages, tuberculous lesions of the tonsils, systemic diseases of the hematopoietic organs, which are accompanied by the formation of necrotic masses in the tonsils, with tumors of the tonsils. Angina of the nasopharyngeal tonsil(acute adenoiditis) is mainly found in children, which is associated with the growth of this tonsil in childhood. The causative agent can be either a virus or a microorganism. In older children with acute adenoiditis, there is a slight violation of the general condition, subfebrile condition, the first symptom is a burning sensation in the nasopharynx, and then the disease proceeds as acute rhinitis, i.e. there is difficulty in nasal breathing, watery, mucous, and subsequently purulent discharge from the nose. There are pains in the ears, nasality, in some cases, the addition of acute otitis media is possible. With pharyngoscopy and posterior rhinoscopy, there is a bright hyperemia of the mucous membrane of the posterior pharyngeal wall, along which mucopurulent discharge flows from the nasopharynx. The nasopharyngeal tonsil increases in size, it is hyperemic, on its surface there are point or continuous raids. In children early age acute adenoiditis begins suddenly with an increase in body temperature up to 40 0 C, often with severe symptoms of intoxication - vomiting, loose stools, symptoms of irritation of the meninges. After 1-2 days, there is difficulty in nasal breathing, nasal discharge, an increase in regional lymph nodes. Complications of adenoiditis - catarrhal or purulent otitis media, retropharyngeal abscess, suppuration of regional lymph nodes. Differential diagnosis in children is carried out with childhood infectious diseases, in which the development of inflammation in the nasopharyngeal tonsil is possible. Treatment, general and local, are carried out according to the same principles as with angina, acute rhinitis. In infancy, it is necessary to prescribe vasoconstrictor nasal drops before each feeding. Less frequent angina are the following. Damage to the side ridges- usually associated with acute adenoiditis or occurs after tonsillectomy. This type of angina is characterized by the appearance at the beginning of the development of the process of pain in the throat with irradiation to the ears. At angina of tubal tonsils(which is also mainly noted in acute inflammatory diseases of the pharynx) a typical symptom, along with sore throats radiating to the ears, is stuffy ears. The correct diagnosis is easy to establish with posterior rhinoscopy. Angina of the lingual tonsil occurs mainly in middle and old age, and the characteristic here is pain when protruding the tongue and its palpation. Diagnosis is made by laryngoscopy. Here it is important to remember such formidable complications of lingual sore throat as edema and stenosis of the larynx, glossitis and phlegmon of the floor of the mouth are sometimes observed. For a general practitioner, it is important to correctly and timely recognize local complications of tonsillitis, requiring consultation and treatment by an otorhinolaryngologist. This is first of all paratonsillitis, which develops a few days after the exacerbation of chronic tonsillitis or tonsillitis has ended. The process is most often localized in the anterior or anteroposterior region between the capsule of the palatine tonsil and the upper part of the anterior palatine arch. Its posterior localization is between the tonsil and the posterior arch, the lower one is between the lower pole and the lateral wall of the pharynx, the lateral one is between the middle part of the tonsil and the lateral wall of the pharynx. Typical in the clinic is the appearance of unilateral pain when swallowing, which, with the development of the process, becomes permanent and sharply increases when swallowing. Trismus occurs - a tonic spasm of the masticatory muscles, speech becomes nasal and indistinct. As a result of regional cervical lymphadenitis, a pain reaction occurs when turning the head. The transition of paratonsillitis from the edematous, infiltrative phase to the abscessing phase usually occurs on the 3rd-4th day. On the 4-5th day, an independent opening of the abscess can occur - either in the oral cavity or in the parapharyngeal space, which leads to the development of a severe complication - parapharyngitis. At the beginning of the disease, before the breakthrough of the abscess, pharyngoscopy reveals asymmetry of the pharynx due to protrusion, most often of the supra-almond region, hyperemia and infiltration of these tissues. In the area of the greatest protrusion, one can often see thinning and yellowish edema - the place of an emerging breakthrough of pus. In unclear cases, a diagnostic puncture is performed. Differential diagnosis is carried out with diphtheria (however, trismus is uncharacteristic for this infection and there are often raids) and scarlet fever, in which a characteristic rash develops, and there are also indications of a typical epidemiological history. Tumor lesions of the pharynx usually occur without fever and severe pain in the throat. With erysipelas, which also occurs without fever and severe sore throat. With erysipelas, which also proceeds without trismus, there is diffuse hyperemia and swelling on the mucous membrane with a brilliant background of the mucous membrane, and with a bullous form, bubbles pour out on the soft palate. Treatment of paratonsillitis in the stage of infiltration and abscessing, surgical - opening of the abscess, its regular emptying, according to indications - abscess-tonsillectomy. The scheme of complex treatment of purulent pathology is given earlier.
Retropharyngeal abscess It usually occurs in young children due to the fact that the retropharyngeal (retropharyngeal) space is filled with loose connective tissue with lymph nodes that are most pronounced in childhood. After 4-5 years, these lymph nodes are reduced. Symptoms- pain when swallowing, which, however, does not reach the same degree as with paratonsillar abscess. In small children, these pains cause severe anxiety, tearfulness, screaming, sleep disturbance, etc. Small patients refuse to breastfeed, cough, spit up milk through the nose, which very soon leads to malnutrition. Further symptoms depend on the reactivity of the organism and the location of the abscess. When it is located in the nasopharynx, respiratory disorders come to the fore, cyanosis appears, inspiratory retraction chest, the voice takes on a nasal tone. With a low position of the retropharyngeal abscess, a narrowing of the entrance to the larynx develops with increasing respiratory failure, which has the character of snoring, which in the future can lead to suffocation. With an even lower location of the abscess, symptoms of compression of the esophagus and trachea appear. When examining the pharynx, one can see a round or oval pillow-shaped swelling of the posterior pharyngeal wall, located on one (lateral) side and giving fluctuation. If the abscess is located in the nasopharynx or closer to the entrance to the larynx, then it is not available for direct viewing, it can only be detected with posterior rhinoscopy or laryngoscopy, or by palpation. With secondary pharyngeal abscesses, these symptoms are accompanied by changes in the spine, the inability to turn the head to the sides, stiff neck. Diagnostic valuable palpation examination. Differential diagnosis is carried out with a tumor of the retropharyngeal space (for example, lipoma), here the puncture will help the correct diagnosis. Treatment surgical.
parapharyngeal abscess This type of abscess is a relatively rare complication of the inflammatory process in the tonsil or near-tonsil tissue. The most common parapharyngeal abscess occurs as a complication of paratonsillar abscess. There is a picture of a long-term non-resolving paratonsillar abscess, when either spontaneous opening of the abscess did not occur, or incision was not performed, or it did not lead to the desired result. The general condition of the patient continues to deteriorate. The temperature is high, leukocytosis increases in the blood, ESR increases. With pharyngoscopy, in some cases, a decrease in swelling and protrusion of the soft palate is noted, but a protrusion of the lateral wall of the pharynx appears in the tonsil area. Protrusions in the parapharyngeal region are accompanied by changes in the neck. Along with enlarged and painful lymph nodes on palpation, a more diffuse and painful swelling appears in the area of the angle mandible(both at the angle of the lower jaw and in the region of the maxillary fossa). If pain along the vascular bundle joins the indicated swelling against the background of a deterioration in the general condition of the patient, then one should think about the beginning of the development of a septic process. The peripharyngeal abscess, which is not opened in a timely manner, entails further complications: sepsis is most common due to involvement of the internal jugular vein in the process. With an abscess in the parapharyngeal space, the process can extend up to the base of the skull. The spread of the process downward leads to mediastinitis. Purulent parotitis may also occur due to a breakthrough in the bed of the parotid gland. Treatment parapharyngeal abscess only surgical.
angina- acute inflammation of the lymphadenoid tissue of the larynx (in the region of the scoop-epiglottic folds, interarytenoid space, in the Morganian ventricles, piriform sinuses and individual follicles). The disease can develop as a result of trauma (in particular, a foreign body), as well as as a complication of SARS. The patient complains of pain when swallowing, soreness when changing the position of the head, dryness in the throat. The phenomena of general intoxication are expressed moderately. Regional lymphadenitis is determined, usually unilateral. Laryngoscopy reveals hyperemia and infiltration of the mucous membrane of the larynx on one side or a limited area. With a protracted course of the process, the formation of abscesses in the places of localization of the lymphoid tissue is possible. Treatment is the same as for acute catarrhal laryngitis, however, in severe cases, massive antibiotic therapy is necessary. With significant stenosis, a tracheostomy is indicated. The patient must follow a regimen that is sparing diet, alkaline inhalations are useful. Anti-inflammatory therapy includes the introduction of sulfonamides, antibiotics into the body; the use of antihistamines is mandatory.
Laryngitis Acute catarrhal laryngitis Acute inflammation of the mucous membrane of the larynx can also be observed as an independent disease (cold, too hot or cold food), chemical or mechanical irritants (nicotine, alcohol, dusty and smoky air), occupational hazards, for example, excessive voice tension (strong cry, loud command ), and with common diseases such as measles, whooping cough, influenza, typhus, rheumatism, etc. Clinical acute laryngitis is manifested by the occurrence of hoarseness, perspiration, soreness in the throat, the patient is worried about dry cough. Violation of the voice is expressed in varying degrees of dysphonia, up to aphonia. The diagnosis of acute laryngitis is not difficult to make based on the history, symptoms, and characteristic hyperemia of the mucous membrane of the larynx. Differential diagnosis should be carried out with false croup (in children) and damage to the larynx in diphtheria, tuberculosis, syphilis. Treatment should primarily include a strict voice mode, a diet with restriction of spicy, hot, cold food, alcohol, smoking. Highly effective inhalations with a solution of antibiotics (fusafungin 2 puffs 4 times a day), with a predominance of the edematous component over the inflammatory component, it is advisable to prescribe inhalations with hydrocortisone or use a beclomethasone dipropionate inhaler 2 puffs 3 times a day, antihistamines are also used, from local treatment - infusions in the larynx of vegetable oil (peach, olive), hydrocortisone suspension.
Phlegmonous (infiltrative-purulent) laryngitis Phlegmonous (infiltrative-purulent) laryngitis is relatively rare - either due to trauma or after an infectious disease (in children - measles and scarlet fever). The submucosal layer is involved in the pathological process, less often the muscular and ligamentous apparatus of the larynx. Patients complain of sharp pain when swallowing, especially when the infiltrate is located in the epiglottis and arytenoid cartilages. Regional lymphadenitis is palpable. Laryngoscopy reveals hyperemia and infiltration of the mucous membrane of the larynx, an increase in the volume of the affected area, sometimes with areas of necrosis. There is a restriction of the mobility of the elements of the larynx. The general inflammatory reaction is expressed. Treatment is carried out in a hospital, taking into account the severity of the picture. With increasing symptoms of stenosis, a tracheostomy is performed. Complex therapy with the inclusion of antibiotics, antihistamines, according to indications - mucolytics is necessary. In the presence of an abscess, its treatment is only surgical in a specialized hospital.
Chondroperichondritis of the cartilage of the larynx The occurrence of this pathology is associated with infection of the cartilage and perichondrium of the skeleton of the larynx as a result of its injury (including after surgical intervention). As a result of the transferred inflammation, necrosis of cartilage tissue, scarring can occur, which leads to deformation of the organ and narrowing of its lumen. The clinical picture is determined by the localization of the inflammatory process and the degree of its development; laryngoscopy reveals a hyperemic area with thickening of the underlying tissues, their infiltration, often with the formation of a fistula. In the treatment, in addition to massive antibiotic therapy and hyposensitization, physiotherapy plays an important role - UV, UHF, microwave, ionogalvanization on the larynx with calcium chloride, potassium iodide. Treatment of chondroperichondritis of the larynx must be carried out in a specialized hospital.
Subglottic laryngitis Subglottic laryngitis (false croup) is a type of acute catarrhal laryngitis that develops in the subglottic space. It is observed in children aged 2-5 years against the background of acute inflammation of the mucous membrane of the nose or pharynx. Clinic false croup is quite characteristic - the disease develops suddenly in the middle of the night, with an attack of barking cough. Breathing becomes wheezing, sharply difficult, inspiratory dyspnea is pronounced. Nails and visible mucous membranes become cyanotic. On examination, retraction of the soft tissues of the jugular fossa, supraclavicular and subclavian spaces is noted. The attack lasts from several minutes to half an hour, after which profuse sweat appears and the condition improves, the child falls asleep. Diagnosis is based on the clinical picture of the disease and laryngoscopy data in cases where it is possible to perform. Differential diagnosis is carried out with true (diphtheria) croup. In the latter case, suffocation develops gradually and does not debut as acute nasopharyngitis. Pronounced regional lymphadenitis. Typical manifestations are dirty gray plaques in the pharynx and larynx. It is necessary to teach the parents of children who have similar conditions, certain tactics of behavior. Usually these are children prone to laryngospasm, suffering from diathesis. General hygienic measures - humidification and ventilation of the air in the room where the child is located; it is recommended to give warm milk, “Borjomi”. Distractions are used: mustard plasters on the neck, hot foot baths (no more than 3-5 minutes). In case of inefficiency, the imposition of a tracheostomy is indicated. Laryngeal edema is not an independent disease, but only one of the manifestations of many pathological processes. Laryngeal edema can be inflammatory and non-inflammatory in nature. Inflammatory edema of the larynx may accompany the following pathological processes: laryngeal tonsillitis, phlegmonous laryngitis, epiglottis abscess, suppurative processes in the pharynx, lateral parapharyngeal and pharyngeal spaces, in the area cervical spine, root of the tongue and soft tissues of the floor of the mouth. One of the common causes of laryngeal edema are injuries - gunshot, blunt, stabbing, cutting, thermal, chemical, foreign bodies. Traumatic laryngeal edema can develop in response to surgery on the larynx and neck, as a result of prolonged upper tracheobronchoscopy, due to prolonged and traumatic intubation of the larynx, after radiation therapy for diseases of the neck. Non-inflammatory laryngeal edema as a manifestation of allergy occurs with idysyncrasy to certain foods, drugs and cosmetics. This also includes angioedema angioedema, in which swelling of the larynx is combined with swelling of the face and neck. Laryngeal edema can develop with diseases of cardio-vascular system accompanied by circulatory failure II-III degree; kidney disease, liver cirrhosis, cachexia. Treatment for laryngeal edema is aimed at treating the underlying disease that led to the edema, and includes dehydration, hyposensitizing and sedatives. First of all, with the inflammatory nature of laryngeal edema, the following appointments are appropriate: 1) parenteral antibiotic therapy (after determining the tolerance of drugs; 2) a solution of promethazine 0.25%, 2 ml per muscle 2 times a day; calcium gluconate solution 10% intramuscularly, depending on the severity of edema; 20 ml of 40% glucose solution, 5 ml of ascorbic acid solution intravenously 1 time per day; rutin 0.02 g orally 3 times a day; 3) hot (42-45 0 C) foot baths for 5 minutes; 4) a warming compress on the neck or mustard plasters for 10-15 minutes 1-2 times a day; 5) when coughing, the appearance of crusts and thick sputum - expectorant and sputum thinners (carbocysteine, acetylcysteine). Inhalations: 1 bottle of chymotrypsin + 1 ampoule of ephedrine + 15 ml of 0.9% sodium chloride solution, breathe 2 times a day for 10 minutes. Treatment should always be carried out in a hospital, as with an increase in difficulty breathing through the larynx, a tracheostomy may be required.
Acute tracheitis
. Usually the disease begins with acute catarrhal rhinitis and nasopharyngitis and quickly spreads downward, covering the trachea, and often large bronchi. In other cases, along with the trachea, large bronchi are also involved in the disease. In this case, the clinical picture becomes acute tracheobronchitis. The most characteristic clinical sign of acute banal tracheitis is a cough, especially disturbing the patient at night and in the morning. With a pronounced inflammatory process, for example, with influenza hemorrhagic tracheitis, the cough is excruciating paroxysmal in nature and is accompanied by a dull sore pain in the pharynx and behind the sternum. Due to pain during deep inspiration, patients try to limit the depth of respiratory movements, which is why breathing quickens to compensate for oxygen deficiency. The general condition of adults at the same time suffers little, sometimes there is subfebrile condition, headache, feeling of weakness, pain throughout the body. In children, the clinical picture is acute with an increase in body temperature up to 39 ° C. Shortness of breath usually does not occur, with the exception of acute severe generalized viral lesions of the upper respiratory tract, in which there is a pronounced general intoxication, impaired cardiac activity, and depression of the respiratory center.
Sputum at the beginning of the disease is scarce, it is difficult to separate, which is explained by the stage of "dry" catarrh. Gradually, it acquires a mucopurulent character, becomes more abundant and is separated more easily. Cough ceases to cause unpleasant scraping pains, the general condition improves.
With the usual clinical course and timely treatment, the disease ends within 1-2 weeks. Under adverse conditions, non-compliance with the prescribed regimen, untimely treatment and other negative factors, recovery is delayed and the process can go into a chronic stage.
Diagnostics acute banal tracheitis does not cause difficulties, especially in cases of seasonal colds or influenza epidemics. The diagnosis is established on the basis of a typical clinical picture and characteristic symptoms of catarrh of the tracheal mucosa. Difficulties arise in influenza toxic forms, when inflammation of the respiratory tract should be differentiated from pneumonia.
Treatment almost identical to that of acute laryngitis. Great importance is attached to the prevention of complications in severe forms of tracheobronchitis, for which the patient is prescribed antibacterial, immunomodulatory, restorative treatment with intensive vitamin (A, E, C) and detoxification therapy. Preventive measures are especially relevant in dusty industries and during periods of influenza epidemics.
Chronic banal tracheitis
Chronic tracheitis is a systemic disease that captures to one degree or another all the respiratory tract, it is a disease of the predominantly adult population of large industrial cities, people who work in hazardous industries and abuse bad habits. Chronic tracheobronchitis can act as complications of childhood infections (measles, diphtheria, whooping cough, etc.), the clinical course of which was accompanied by acute tracheitis and bronchitis.
Symptoms and clinical course. The main symptom of chronic tracheitis is a cough, which is more severe at night and in the morning. This cough is especially painful when sputum accumulates in the carina area, which dries up into dense crusts. With the development of an atrophic process, in which only the surface layer of the mucous membrane is affected, the cough reflex persists, however, with deeper atrophic phenomena that involve nerve endings as well, the severity of cough decreases. The course of the disease is long, alternating with periods of remission and exacerbation.
Diagnosis established by fibroscopy. However, the cause of this disease often remains unknown, except in those cases when it occurs in persons of harmful professions.
Treatment determined by the type of inflammation. With hypertrophic tracheitis, accompanied by the release of mucopurulent sputum, inhalation of antibiotics is used, the selection of which is carried out on the basis of an antibiogram, inhalation of astringent powders at the time of inhalation. In atrophic processes, vitamin oils are instilled into the trachea (carotolin, rosehip and sea buckthorn oil). The crusts are removed by infusion into the trachea of solutions of proteolytic enzymes. Basically, the treatment corresponds to that of banal laryngitis.
Inflammatory diseases of the esophagus include:
Acute esophagitis.
Chronic esophagitis.
Reflux esophagitis.
Peptic ulcer of the esophagus.
The last two diseases are the result of systematic irritation of the esophageal mucosa by the acidic contents of the stomach, causing inflammation and tissue degeneration.
Acute esophagitis.
Acute acute esophagitis occurs as a result of an acute bacterial or viral infection. They have no practical significance during the course of the disease and disappear along with other signs of the disease, if they do not acquire an independent chronic course.
Acute esophagitis can be:
Catarrhal esophagitis.
Hemorrhagic esophagitis.
Purulent esophagitis (abscess and phlegmon of the esophagus).
The causes of acute esophagitis are chemical burns (exfoliative esophagitis) or trauma (bone splinter, injury when swallowing sharp objects, bones).
Clinical picture acute esophagitis. Patients complain of acute esophagitis on pain behind the sternum, aggravated by swallowing, sometimes there is dysphagia. The disease occurs acutely. It is also accompanied by other features characteristic of the main process. With influenza, this is fever, headache, sore throat, etc. With a chemical burn, there are indications of ingestion of alkali or acid, traces of a chemical burn are found on the oral mucosa, in the pharynx. An abscess or phlegmon of the esophagus is characterized by severe pain behind the sternum when swallowing, difficulty in swallowing dense food, while warm and liquid food does not linger in it. There are signs of infection and intoxication - fever, leukocytosis in the blood, ESR is increased, proteinuria occurs.
X-ray examination allows you to detect an infiltrate that causes some delay in the food bolus, to establish its localization and the degree of damage to the esophageal wall.
Esophagoscopy: mucosa in the infiltrate area is hyperemic, edematous. With careful examination, you can find a splinter - a fish bone or a sharp bone stuck in the tissue of the esophagus. The foreign body is removed using forceps. It is possible to feel the density of the infiltrate with the edge of the apparatus. If the abscess has matured, a tissue of soft consistency is revealed in the center.
Diffuse esophagitis accompanied by hyperemia and mucosal edema. It is covered with a white-gray coating, bleeds easily. Erosions have an irregular shape, often longitudinal, covered with a gray coating. Peristalsis is preserved.
Acute esophagitis can occur without consequences. After a chemical burn, powerful scars develop, causing a narrowing of the esophagus.
Inflammation of the mucous membrane of the posterior pharyngeal wall - pharyngitis- can be acute or chronic.
Acute pharyngitis
- Acute inflammation of the mucous membrane is rare, as an independent disease. More often it is a consequence of a respiratory viral infection or the result of the spread of bacterial flora from the nasal cavity, from the tonsils or carious teeth.
The reasons, contributing to the development of pharyngitis, may be the following:
General or local hypothermia;
Irritation of the mucous membrane with secretions flowing from the paranasal sinuses;
exposure to harmful impurities in the air - dust, gases, tobacco smoke;
Acute infectious diseases;
Diseases internal organs- kidneys, blood, gastrointestinal tract, etc.
Clinical manifestations acute pharyngitis the following:
Dryness, perspiration, sore throat;
Moderate pain when swallowing;
Irradiation of pain in the ear;
Hearing loss - "congestion" of the ears, clicking in the ears when the process spreads to the nasopharynx and the mouth of the auditory tubes;
Mild signs of intoxication, subfebrile temperature.
With oropharyngoscopy notes:
Hyperemia and moderate swelling of the posterior pharyngeal wall;
Thickened hyperemic follicles, edematous lateral ridges;
Muco-purulent discharge on the back of the pharynx in the presence of a bacterial pathogen.
Expressed forms of acute pharyngitis are accompanied by regional lymphadenitis.
Treatment acute pharyngitis includes:
Sanitation of foci of infection in the nasal cavity, nasopharynx,
oral cavity, tonsils;
Elimination of annoying factors;
Gentle diet;
Plentiful warm drink;
Warm-moist inhalations with the addition of essential oils, soda;
Irrigation of the back wall with warm disinfectant solutions: furacillin, chlorophyllipt, hexoral, povidone iodine, herbal decoctions;
Aerosol preparations: "Kameton", "Ingalipt", "Proposol", IRS19;
Oroseptics for resorption in the oral cavity "Faringosept", "Septolete", "Strepsils", "Lariprokt", "Lariplus", etc.
Lubrication of the back wall of the pharynx with oil solutions, Lugol's solution;
Antiviral agents: interferon, rimantadine, etc.
Prevention consists of the following activities:
hardening procedures;
Restoration of nasal breathing;
Elimination of annoying factors.
Chronic pharyngitis
depending on the nature
inflammatory process is divided into catarrhal(simple), hypertrophic(granular and lateral) and atrophic and combined(mixed). The reasons development of chronic pharyngitis:
External irritating factors;
The presence of foci of infection in the nose, paranasal sinuses, oral cavity and tonsils;
Violation of metabolic processes (diathesis in children, diabetes in adults, etc.);
Stagnation in diseases of the internal organs.
Subjective signs various forms of pharyngitis are largely identical:
Dryness, burning, itching in the throat
Soreness with an "empty throat";
Feeling foreign body;
Irradiation of pain in the ears;
Accumulation of viscous mucous discharge, especially
in the morning.
Diagnosis of chronic pharyngitis It is put mainly on the basis of pharyngoscopy data:
- with catarrhal there is hyperemia of the mucous membrane, its thickening, increased vascular pattern;
- with hypertrophic form- on the swollen and hyperemic mucosa of the posterior pharyngeal wall, individual red grains (granules), an increase and swelling of the lateral ridges are visible;
- with atrophic form the mucous membrane is dry, thinned, shiny, pale, sometimes covered with viscous mucus or crusts.
Treatment depends on the form and stage of the disease and, above all, should be aimed at eliminating the causes of the disease.
Local treatment consists in the appointment of irrigation, inhalation, spraying and lubrication with drugs corresponding to the form of the disease. With atrophic pharyngitis use alkaline and oil preparations. With hypertrophic pharyngitis the mucous membrane is treated with a 1-5% solution of collargol, protargol or lapis, novocaine blockade. For severe hypertrophy, cryotherapy(freezing) on granules and side rollers.
The result of treatment with these methods often does not satisfy the doctor and the patient. In recent years, a new method for the treatment of acute and chronic pharyngitis has appeared, which consists in the use of vaccines, which are lysates of pathogens of the upper respiratory tract. Such a drug is Imudon, which is produced in France and is widely used to treat diseases of the oral cavity and pharynx. The drug is available in tablets for resorption in the oral cavity. Imudon has a local effect on the mucous membrane, which results in an increase in phagocytic activity, the amount of secretory immunoglobulin A, and an increase in the content of lysozyme in saliva. The maximum effect in the treatment of this drug in the form of monotherapy and in combination with other drugs is obtained in acute and chronic catarrhal and hypertrophic pharyngitis. Successful use of Imudon for specific prevention and treatment inflammatory diseases oral cavity plays a significant role in the prevention of diseases of the pharynx. Studies have shown that the use of Imudon in the treatment of frequently ill children leads to an increase in the content of interferon in saliva, a decrease in the number of exacerbations of diseases and a decrease in the need for antibiotic therapy.
Acute tonsillitis (tonsillitis)- This is a common infectious-allergic disease with an inflammatory process in the lymphoid tissue of the palatine tonsils. Inflammation can also occur in other accumulations of lymphoid tissue of the pharynx - lingual, pharyngeal, tubal tonsils, in the lateral ridges. To define these diseases, the term is used - angina, (from the Latin Anqo - to compress, choke), known since ancient times. In Russian medical literature, you can find the definition of angina, as "throat toad." The disease mainly affects children of preschool and school age as well as adults under the age of 40. There are pronounced seasonal rises in the incidence in the spring and autumn periods.
There are several classification schemes for angina. They are distinguished by etiology, pathogenesis, clinical course.
Among the various microbial pathogens, the main etiological role belongs beta-hemolytic streptococcus, which is found according to different authors from 50 to 80% of cases. The second most common causative agent of angina can be considered golden staphylococcus. Diseases caused by green streptococcus. In addition, the causative agent of angina can be adenoviruses, rods, spirochetes, fungi and others
The penetration of an exogenous pathogen can occur by airborne droplets, alimentary and by direct contact with a patient or bacillus carrier. More often, the disease occurs due to autoinfection with microbes or viruses that normally vegetate on the mucous membrane of the pharynx. It is possible to spread an endogenous infection from carious teeth, a pathological focus in the paranasal sinuses, etc. In addition, tonsillitis can occur as a relapse of a chronic process.
According to classification by I.B. Soldatova(1975) acute tonsillitis (tonsillitis) are divided into two groups: primary and secondary,
To primary(banal) tonsillitis include - catarrhal, follicular, lacunar, phlegmonous tonsillitis.
Secondary(specific) tonsillitis caused by a specific specific pathogen. They can be a sign of an infectious disease (diphtheria of the pharynx, ulcerative necrotic tonsillitis, syphilitic, herpetic, fungal) or blood diseases.
Primary (banal) tonsillitis
Catarrhal tonsillitis- the mildest form of the disease, having the following Clinical signs;
Burning sensation, dryness, sore throat;
Soreness when swallowing is mild;
Subfebrile temperature;
Moderately expressed intoxication;
Enlargement of regional lymph nodes;
The duration of the disease is 3-5 days.
With pharyngoscopy defined:
Diffuse hyperemia of the tonsils and palatine arches;
Slight enlargement of the tonsils;
In places, a film of mucopurulent exudate is determined.
Follicular tonsillitis has the following features:
The onset is acute with an increase in temperature to 38-39 °;
Severe pain in the throat when swallowing;
Irradiation of pain in the ear;
Intoxication is pronounced, especially in children - loss of appetite, vomiting, confusion, meningism phenomena;
Significant hematological changes - neutrophilic leukocytosis, stab shift, accelerated ESR;
Enlargement and soreness of regional lymph nodes.
The duration of the disease is 5-7 days. With pharyngoscopy defined:
Severe hyperemia and infiltration of the soft palate and arches;
Enlargement and hyperemia of the tonsils, bumpy surface in the first days of the disease;
Multiple yellowish-white dots 1-3 mm in size (purulent follicles) 3-4 days of illness.
Lacunar tonsillitis often proceeds more severely than follicular. Inflammation develops, as a rule, in both tonsils, however, on one side there may be a picture of follicular tonsillitis, and on the other - lacunar. This is explained by a deeper lesion of all lymphoid follicles. Superficially located follicles give a picture of follicular tonsillitis. The follicles located in the depth of the tonsil fill the adjacent lacunae with their purulent contents. With an extensive process, pus comes to the surface of the tonsil in the form of islets or drain raids.
Clinical signs lacunar tonsillitis are as follows:
Severe pain in the throat when swallowing food and saliva;
Irradiation of pain in the ear;
Chills, fever up to 39-40°;
Weakness, fatigue, sleep disturbance, headache;
Pain in the lower back, joints, in the region of the heart;
Pronounced hematological changes;
Significant enlargement and soreness of regional lymph nodes and spleen.
The duration of the disease is 10-12 days.
At pharyngoscopy are defined:
Severe hyperemia and enlargement of the tonsils;
Yellowish-white plaques located at the mouths of lacunae, which are easily removed with a spatula;
Islands of purulent raids, sometimes covering a significant surface of the tonsil.
Phlegmonous
tonsillitis is relatively rare and is characterized by purulent fusion of tissue inside the tonsil - phlegmon formation.
The reasons, contributing to the formation of the process can be the following:
Decreased immune forces of the body;
Virulence of the pathogen;
Injury to the tonsil by a foreign body or during medical procedures;
The development of adhesions in the depth of the tonsil with difficulty in the outflow of contents.
Clinical signs phlegmonous tonsillitis may be similar to manifestations of lacunar tonsillitis, small abscesses may be almost asymptomatic. In more severe cases, there is an increase in pain on the one hand, difficulty in swallowing, worsening of the general condition.
With pharyngoscopy defined:
Enlargement of one tonsil, hyperemia, tension;
Pain when pressed with a spatula;
The presence of fluctuations in mature phlegmon.
The submandibular lymph nodes are enlarged and painful on the side of the lesion.
Treatment of primary (banal) tonsillitis should be etiotropic, complex - local and general. As a rule, treatment is carried out at home, and only in severe cases or under adverse social conditions the patient is placed in a hospital. To confirm the diagnosis and select the appropriate treatment, bacteriological examination contents of the nose and throat. Treatment should include the following steps:
1. Treatment adherence diseases:
Strict bed rest during the first days of the disease;
Sanitary and epidemic standards - isolation of the patient, individual care products and personal hygiene items;
Diet - mechanically, thermally and chemically sparing diet, rich in vitamins, drink plenty of water.
2. Local treatment:
- gargling with warm solutions of potassium permanganate, furacillin, gramicidin, sodium bicarbonate, chlorophyllipt, hexoral, povidone iodine, as well as decoctions of chamomile, sage, eucalyptus;
Treatment of the mucous membrane of the pharynx with aerosol preparations: "Kameton", "Eucalyptus", "Proposol", "Bioparox";
The use of oroseptics: "Faringosept", "Geksaliz", "Lari-plus", "Laripront", "Septolete", "Strepsils", "Anti-Angin", etc.;
Lubrication of the pharyngeal mucosa with Lugol's solution, iodinol;
Aromatherapy: essential oils eucalyptus, cedar, tea tree, lavender, grapefruit. 3. General treatment:
Sulfanilamide drugs are prescribed taking into account the severity of the course of the disease, usually in the initial stage;
Antihistamines are recommended due to the toxic-allergic nature of the disease (tavegil, suprastin, diazolin, phenkarol, etc.). Antibacterial therapy is prescribed depending on the severity and stage of the disease: young people in initial stage disease, the use of antibiotics is not recommended. AT severe cases, in the stage of abscess formation or in case of damage to other organs, apply semi-synthetic broad-spectrum drugs(ampicillin, amoxicillin, amoxiclav, unazine), first generation cephalosporins(cephalexin, cephalothin, cephalosin), macrolides(erythromycin, rovamycin, rulid). Treatment with antibiotics should be accompanied by the prevention of dysbacteria for - the appointment of nystatin, levorin, diflucan. With the wrong choice of antibiotics and the timing of treatment, conditions are created for the process to become chronic.
Anti-inflammatory drugs - paracetamol, acetylsalicylic acid are prescribed for hyperthermia, and it is necessary to take them into account side effects;
Immunostimulating therapy is recommended in the form of the following drugs: extract thymus(vilozen, timoptin), pyrogenal, natural immunostimulants (ginseng, leuzea, chamomile, propolis, pantocrine, garlic). The use of a vaccine-type immunomodulator - the drug Imudon - gives positive results in the treatment of herpetic, fungal lesions of the oral cavity and pharynx, increases phagocytic activity and the level of lysozyme in saliva.
Physiotherapy procedures are prescribed after the removal of hyperthermia and the elimination of the purulent process with prolonged lymphadenitis: solux, UHF on the submandibular region, phonophoresis, magnetotherapy.
In the process of treatment, it is necessary to monitor the state of the cardiovascular system, to conduct repeated studies of urine and blood. After the illness, the patient should be under the supervision of a doctor for a month.
Prevention of acute tonsillitis should include:
Timely rehabilitation of foci chronic infection;
Removing the causes that hinder nasal breathing;
Exclusion of irritating factors in the environment;
The correct mode of work and rest, tempering procedures.
Persons who often suffer from angina are subject to dispensary observation.
Paratonsillitis in most cases, it is a complication of tonsillitis in patients with chronic tonsillitis and occurs as a result of the penetration of a virulent infection into the peri-almond tissue. The reasons for the development of paratonsillitis in most cases are a decrease in immunity and inadequate or early discontinued treatment of angina. The spread of the inflammatory process beyond the capsule of the tonsil indicates the termination of its protective action, that is, the transition to the stage of decompensation.
Clinical manifestations of the disease:
Constant pain when swallowing, aggravated by trying to swallow saliva;
Irradiation of pain in the ear, teeth, aggravated to the refusal of food and drink;
emergence trismus- spasm of chewing muscles;
Slurred, nasal speech;
Forced position of the head (sideways), resulting from inflammation of the muscles of the pharynx, neck and cervical lymphadenitis;
Severe intoxication - headache, feeling of weakness, febrile temperature;
Significant hematological changes of an inflammatory nature.
Pharyngoscopy usually difficult due to lockjaw, on examination there is an unpleasant putrid odor from the mouth. A characteristic picture is the asymmetry of the soft palate due to the displacement of one of the tonsils to the midline. Depending on the location of the abscess in the peri-almond tissue, anterior-upper, antero-inferior, lateral and posterior peri-almond abscesses are isolated. With anterior superior paratonsillitis, there is a sharp bulging of the upper pole of the tonsil, which, together with the arches and the soft palate, is a spherical formation. In the region of greatest protrusion, fluctuation.
During the course of the disease, there are two stages - infiltration and abscess formation. To resolve the issue of the presence of pus, a diagnostic puncture is performed.
Treatment paratonsillitis in infiltrative stage carried out according to the scheme recommended for acute tonsillitis. The complex nature of the treatment, the use of broad-spectrum antibiotics, the appointment of novocaine blockades can lead to a gradual attenuation of the inflammatory process and recovery of the patient.
When an abscess matures do not wait for its spontaneous emptying. It is desirable to perform an autopsy after spraying the pharyngeal mucosa with a 10% solution of lidocaine or a 2% solution of dicaine. The introduction of 2-3 ml of a 1% solution of novocaine into the area of masticatory muscles near the angle of the lower jaw removes trismus and facilitates manipulation. The opening of the abscess is often done through. supra-almond fossa or at the site of the greatest protrusion with a scalpel or forceps. In the following days, the wound edges are diluted, its cavity is washed with disinfectants.
To prevent possible relapses of the process and the development of complications, the patient is removed the tonsils - tonsillectomy. Usually, the operation is performed a week after the opening of the paratonsillar abscess. In some cases, in the presence of chronic tonsillitis complicated by paratonsillitis, as well as when other complications are detected, the entire purulent focus is removed at any location, which ensures a quick recovery of the patient.
Retropharyngeal abscess is a purulent inflammation of the lymph nodes and loose tissue between the fascia of the pharynx and the prevertebral fascia, which persist in children up to the age of four. At a younger age, the disease occurs as a result of the introduction of infection into the pharyngeal space with acute rhinopharyngitis, tonsillitis, acute infectious diseases against a background of weakened immunity. In older children, the cause of the retropharyngeal abscess is often trauma to the posterior pharyngeal wall.
Clinical manifestations of the disease depend on the localization of the abscess, its size, the state of immunity, the age of the child. However, the disease is always severe, and the leading symptoms are sore throat and difficulty breathing:
- at a high position an abscess in the nasopharynx marked difficulty in nasal breathing, nasality;
- at an average location abscess appears noisy stridor breathing, snoring, voice becomes hoarse;
- when lowering an abscess into the laryngopharynx, breathing becomes stenotic, with the participation of auxiliary muscles, cyanosis is noted, occasional attacks of suffocation, forced head position with tilting back;
Sore throat, food refusal, anxiety and fever are characteristic of all types of process localization.
With pharyngoscopy there is hyperemia and swelling of a rounded shape on the back of the pharynx along the midline or occupying only one side. With a pronounced trismus in young children, a digital examination of the nasopharynx and oropharynx is performed, in which an infiltrate of a dense consistency or fluctuating is found. Regional The lymph nodes greatly enlarged and painful.
Treatment. In the stage of infiltration is assigned conservative treatment. When signs of abscess appear, surgical intervention - opening of the abscess, which is carried out in order to prevent aspiration horizontal position with preliminary puncture and suction of pus. An incision is made at the site of the greatest protrusion, immediately after a deep breath, and the child's head is lowered down. After opening, the edges of the wound are re-diluted, the throat is irrigated with disinfectants, and antibacterial treatment is continued.
Secondary (specific) tonsillitis are signs of blood diseases or are caused by pathogens of infectious diseases.
Ulcerative membranous (necrotic) angina Simanovsky-Vincent caused by bacterial symbiosis fusiform rods and spirochetes of the oral cavity, are usually in a low-virulence state in the folds of the oral mucosa. Factors predisposing to the development of the disease are:
Decreased general and local reactivity of the body;
Transferred infectious diseases;
The presence of carious teeth, gum disease.
Clinical manifestations, diseases are as follows:
Body temperature rises to subfebrile figures or may remain normal;
There are no pains in the throat, there is a feeling of awkwardness, a foreign body when swallowing;
Putrid smell from the mouth, increased salivation.
With pharyngoscopy pathological changes are found on one tonsil:
In the upper pole there is a grayish or yellowish coating;
After rejection of the plaque, a deep ulcer is formed with uneven edges and a loose bottom.
Regional nodes are enlarged on the affected side,
moderately painful.
The duration of the disease is from 1 to 3 weeks.
Treatment ulcerative necrotic tonsillitis is carried out in the infectious department of the hospital. Upon admission, a bacteriological examination is performed to clarify the diagnosis.
Local treatment includes:
Cleansing the ulcer from necrosis with a 3% solution of hydrogen peroxide;
Irrigation of the pharynx with a solution of potassium permanganate, furacilin;
Lubrication of the ulcer with tincture of iodine, a mixture of 10% suspension of novarsenol in glycerin;
primary stage syphilis in the pharynx can occur during oral sex, with the following clinical manifestations:
Slight pain when swallowing on the side of the lesion;
On the surface of the tonsil, red erosion is determined, an ulcer or tonsil takes on the appearance, as in acute tonsillitis;
The tissue of the tonsil is dense when palpated;
There is a unilateral increase in lymphatic
nodes.
Secondary syphilis The pharynx has the following characteristic features:
Spilled copper-red color of the mucous membrane, exciting arches, soft and hard palate;
Papular rash, round or oval, grayish-white;
Enlargement of regional lymph nodes.
Tertiary syphilis appears as a limited
gummy tumor, which, after disintegration, forms a deep ulcer with smooth edges and a greasy bottom with further destruction of surrounding tissues if left untreated.
Treatment specific, locally prescribed rinsing with disinfectant solutions (see section "Chronic specific diseases of the ENT organs").
Herpetic tonsillitis refers to diseases caused by adenoviruses. The causative agent of herpangina is the Coxsackie virus of group A. The disease is epidemic in nature, in summer and autumn, and is highly contagious. Children are more commonly affected, especially younger ones.
Clinical manifestations the following:
Increasing the temperature to 38~40 o C;
Pain in the throat when swallowing;
Headache, muscle pain in the abdomen;
vomiting and liquid stool seen in young children.
In adults, the disease occurs in a milder form.
With pharyngoscopy defined:
Hyperemia of the mucous membrane of the pharynx;
Small vesicles on a hyperemic base in the area of the soft palate, uvula, palatine arches, sometimes on the posterior wall of the pharynx;
The formation of ulcers at the site of the opened vesicles on the 3rd-4th day of the disease.
Treatment carried out at home and includes:
Isolation of the patient from others, compliance with the sanitary and hygienic regime;
Sparing diet, plentiful drink, rich in vitamins;
Irrigation of the pharynx with solutions of potassium permanganate, furacilin, povidone iodine;
Treatment antiviral agents(interferon);
Anti-inflammatory therapy (paracetamol, nurofen, etc.) .);
Detoxification therapy is indicated in young children in severe cases, which requires hospitalization.
Fungal tonsillitisin has recently become widespread in the following reasons:
Reduced immunity in the general population;
Failure immune system in children of early
age;
Transferred serious diseases that reduce the nonspecific defenses of the body and change the composition of the microflora of hollow organs;
Long-term use of drugs that suppress the body's defenses (antibiotics, corticosteroids, immunosuppressants).
On bacteriological examination fungal tonsillitis, pathogenic yeast-like fungi such as Candida are found.
Characteristic clinical manifestations the following:
The rise in temperature is not constant;
Minor sore throat, dryness, impaired taste sensations;
The phenomena of general intoxication are poorly expressed.
With pharyngoscopy defined:
Enlargement and slight hyperemia of the tonsils, bright white, loose curd-like plaques that are easily removed without damaging the underlying tissue.
Regional lymph nodes are enlarged, painless.
Treatment is carried out as follows:
Cancellation of broad-spectrum antibiotics;
Irrigation of the pharynx with a solution of chinosol, iodinol, hexoral, povidone iodine;
Insufflation of nystatin, levorin;
Lubrication of the affected areas with 2% aqueous or alcoholic solutions of aniline dyes - methylene blue and gentian violet, 5% solution of silver nitrate;
Nystatin, levorin, diflucan orally in a dosage appropriate for age;
Large doses of vitamins C and group B;
Immunostimulating drugs, imudon;
Ultraviolet irradiation of the tonsils.
Angina with infectious mononucleosis characterized by the following signs;
Chills, fever up to 39~40 C, headache
pain;
An increase in the palatine tonsils, a picture of lacunar, sometimes ulcerative necrotic tonsillitis;
Enlargement and soreness of the cervical, submandibular lymph nodes;
Simultaneous enlargement of the liver and spleen;
When examining blood, an increase in the number of mononuclear cells and a shift in the formula to the left.
Treatment patients is carried out in the infectious diseases department, where it is prescribed:
Bed rest, food rich in vitamins;
- local treatment: rinsing with disinfectants and
astringents;
- general treatment: administration of antibiotics to eliminate secondary infection, corticosteroids.
Agranulocytic angina
is one of the characteristic signs of agranulocytosis and has the following
clinical manifestations:
Chills, high temperature - up to 4 CGS, general serious condition;
Severe sore throat, refusal to eat and drink;
Necrotic dirty gray plaque covering the mucous membrane of the pharynx and oral cavity;
Unpleasant putrid odor from the mouth;
Spread of the necrotic process into the depths of the tissues;
In the blood, there is a pronounced leukopenia and a pronounced shift of the leukocyte formula to the right.
Treatment carried out in the hematology department:
Bed rest, sparing diet;
Careful oral care;
Appointment of corticosteroids, pentoxyl, vitamin therapy;
Bone marrow transplantation;
Fight against secondary infection.
Chronic tonsillitis. This diagnosis refers to chronic inflammation of the palatine tonsils, which is more common than inflammation of all other tonsils combined. The disease usually affects children of school age from 12 to 15% and adults under 40 years old - from 4 to 10%. The basis of this pathology is an infectious-allergic process, which is manifested by repeated tonsillitis and causes damage to many organs and systems. Therefore, knowledge of the symptoms of the disease, its timely detection and rational treatment will help prevent complications in patients and the need for surgical intervention.
The reasons the development of a chronic inflammatory process in the palatine tonsils are the following:
Change in the reactivity of the body;
Difficulty in nasal breathing due to the curvature of the nasal septum, hypertrophy of the turbinates, enlargement of the adenoids;
Chronic focal infection (sinuitis, adenoiditis, carious teeth), which is the source of the pathogen and contributes to the occurrence of relapses of angina;
Transferred childhood infections, repeated respiratory viral diseases, infections of the gastrointestinal tract, which reduce the body's resistance;
The presence of deep lacunae in the palatine tonsils, creating favorable conditions for the development of virulent microflora;
Assimilation of foreign protein, microflora toxins and tissue decay products in lacunae, contributing to local and general allergization of the body;
Extensive lymphatic and circulatory pathways, leading to the spread of infection and the development of complications of an infectious-allergic nature.
Chronic tonsillitis should be attributed to the actual infectious diseases, due in the majority autoinfection. According to the latest data
foreign and domestic publications in the etiology of chronic tonsillitis, the leading place is occupied by group A beta-hemolytic staphylococcus aureus- in children 30%, in
adults 10-15%, then Staphylococcus aureus, hemolytic staphylococcus aureus, anaerobes, adenoviruses, herpes virus, chlamydia and toxoplasma.
The variety of local and general signs of chronic tonsillitis and their relationship with other organs made it necessary to systematize these data. There are several classifications of chronic tonsillitis. Currently the most widely accepted classification by I.B. Soldierea(1975), dividing chronic tonsillitis into specific(syphilis, tuberculosis, scleroma) and nonspecific, which in turn is divided into compensated and decompensated form. According to the well-known classification of B.S. Preobrazhensky, a simple form of chronic tonsillitis and a toxic-allergic form are distinguished.
The basis for setting diagnosis chronic tonsillitis are frequent sore throats in history, local pathological signs and general toxic-allergic phenomena. It is advisable to evaluate the objective signs of chronic inflammation of the palatine tonsils no earlier than 2-3 weeks after the exacerbation of the disease.
Compensated form of chronic tonsillitis characterized by the following features: Patient complaints:
Sore throat in the morning, dryness, tingling;
Feeling of awkwardness or foreign body when swallowing;
Bad smell from mouth;
An indication of angina in history.
Data pharyngoscopy (local signs) inflammatory process in the pharynx:
Changes in the arches - hyperemia, roller-like thickening and swelling of the edges of the anterior and posterior arches;
Spikes of the palatine arches with tonsils as a result of repeated tonsillitis;
Uneven coloring of the tonsils, their looseness, pronounced lacunar pattern;
The presence of purulent-caseous plugs in the depths of lacunae or liquid creamy pus, which are detected by pressing with a spatula on the basis of the anterior palatine arch;
Hypertrophy of the palatine tonsils in chronic tonsillitis, which occurs mainly in children;
Enlargement and soreness of regional lymph nodes in the submandibular region and along the anterior edge of the sternocleidomastoid muscle is a characteristic sign of the disease.
The presence of 2-3 of the listed signs gives grounds for the diagnosis. With a compensated form of the disease in the period between tonsillitis, the general condition is not disturbed, there are no signs of intoxication and allergization of the body.
Decompensated form chronic tonsillitis is characterized by the above local features pathological process in the palatine tonsils, the presence of exacerbations 2-4 times a year, as well as common manifestations of decompensation:
The appearance of subfebrile temperature in the evenings;
Increased fatigue, decreased performance;
Periodic pain in the joints, in the heart;
functional disorders nervous, urinary and other systems;
The presence, especially during periods of exacerbation, diseases associated with chronic tonsillitis- having a common etiological factor and mutual
action on each other. Such diseases of an infectious-allergic nature include: acute and
chronic tonsillogenic sepsis, rheumatism, infectious arthritis, diseases of the heart, urinary system, meninges and other organs and systems.
Local complications that occur in the pharynx against the background of repeated tonsillitis are evidence of decompensation of the inflammatory process in the pharynx, these include: paratonsillitis, pharyngeal abscess.
Accompanying illnesses do not have a single etiological and pathogenetic basis with chronic tonsillitis, the connection is through general and local reactivity. An example of such diseases can be: hypertension, hyperthyroidism, diabetes mellitus, etc.
Treatment of chronic tonsillitis.a due to the form of the disease compensated form held conservative treatment, at decompensated form recommended surgical intervention- tonsillectomy- complete removal of the palatine tonsils.
Conservative treatment chronic tonsillitis should be complex - local and general. It should be preceded by sanitation of foci of infection in the oral cavity, nasal cavity and paranasal sinuses.
Local treatment includes the following activities:
1. Washing the lacunae of the tonsils and rinsing with antiseptic solutions (furacillin, iodinol, dioxidine, chinosol, octenisept, ectericide, chlorhexidine, etc.) on
a course of 10-15 procedures. Washing the gaps with interferon stimulates the immunological properties of the tonsils.
2. Quenching the lacunae of the tonsils with Lugol's solution or 30% alcohol tincture of propolis.
3. Introduction to the Lacunas of antiseptic ointments and pastes on a paraffin-balsamic basis.
4. Intramindal novocaine blockades.
5. The introduction of antibiotics and antiseptic drugs in accordance with the sensitivity of the flora.
6. The use of local immunostimulating drugs: levamisole, dimexide, splenin, IRS 19, ribomunil, Imudon, etc.
7. Reception of oroseptics: pharyngosept, hexalysis, lariplyus, neoangin, septolete, etc.
8. Treatment with the Tonsilor apparatus, which combines ultrasonic action on the tonsils, aspiration of pathological contents from the lacunae and pockets of the tonsils, and irrigation with antiseptic solutions. The course of treatment consists of 5 sessions every other day.
9. Physiotherapeutic methods of treatment: ultraviolet irradiation, phonophoresis of lidase, vitamins, UHF, laser therapy, magnetotherapy.
10. Aromatherapy: essential oils of eucalyptus, cedar, tea tree, lavender, grapefruit, etc.
General therapy chronic tonsillitis is carried out as follows:
1. Antibiotic therapy is used for exacerbation of chronic tonsillitis after determining the sensitivity of the microflora. Treatment with antibiotics should be accompanied by the prevention of dysbacteriosis.
2. Anti-inflammatory therapy is prescribed for an acute process with a hyperergic reaction (paracetamol, aspirin, etc.)
3. Antihistamines are prescribed to prevent complications of an infectious-allergic nature.
4. Immunostimulating therapy should be carried out both during an exacerbation and outside it. Thymus gland extract preparations are prescribed: thymalin, timoptin, vilozen, tim-uvokal; immunocorrectors of microbial origin; natural immunostimulants: ginseng,
echinocea, propolis, pantocrine, chamomile, etc.
5. Antioxidants, the role of which is to improve metabolism, the functioning of enzyme systems, increase immunity: routine-containing complexes, vitamins of groups A, E, C, trace elements - Zn, Mg, Si, Fe, Ca.
The treatment described above is carried out 2-3 times a year, more often in the autumn-spring period, and gives a high therapeutic effect.
The criterion for the effectiveness of treatment is:
1. Disappearance of pus and pathological contents in the palatine tonsils.
2. Reducing hyperemia and infiltration of the palatine arches and tonsils.
3. Reduction and disappearance of regional lymph nodes.
In the absence of these results or the occurrence of exacerbations of the disease, it is indicated tonsillectomy.
Treatment of the decompensated form chronic tonsillitis is carried out surgically with complete removal of the tonsils along with the adjacent capsule.
Contraindication for tonsillectomy is:
Severe degree cardiovascular insufficiency;
Chronic kidney failure;
blood diseases;
Severe diabetes mellitus;
High degree of hypertension with possible development
hypertensive crises, etc.
In such cases, semi-surgical methods of treatment are used. (cryotherapy freezing of tonsil tissue) or conservative treatment.
Preparing for the operation performed on an outpatient basis and includes:
Sanitation of foci of infection;
Blood test for coagulability, content
platelets, prothrombin index;
Measurement of blood pressure;
Examination of internal organs.
The operation is performed on an empty stomach under local anesthesia using a special set of instruments.
The most frequent complication tonsillectomy is bleeding from the area of the tonsil niches.
Patient care in the postoperative period the nurse should carry out as follows: - lay the patient on his right side on a low pillow;
prohibit getting up, actively moving in bed and talking;
Put a diaper under the cheek and ask the patient not to swallow, but to spit saliva;
Observe the patient's condition and saliva color for two hours;
Inform the doctor about the presence of bleeding if necessary;
Give a few sips of cold liquid in the afternoon;
Feed the patient liquid or pureed, cool food for 5 days after surgery;
Irrigate the throat several times a day with aseptic solutions.
Prevention chronic tonsillitis is as follows:
Pollution control;
Improving hygienic working and living conditions;
Improving the socio-economic standard of living of the population;
Active identification of persons suffering from chronic tonsillitis and dispensary observation of them;
Timely isolation of patients and the appointment of adequate treatment;
Individual prophylaxis consists in the sanitation of foci of infection and increasing the body's resistance to the harmful effects of the external environment.
Clinical examination patients with chronic tonsillitis
is effective method recovery of the population. Main goals clinical examinations in otorhinolaryngology are as follows:
Timely detection of patients with chronic and often recurrent diseases;
Systematic monitoring of them and active treatment;
Identification of the causes of this disease, and the implementation of recreational activities;
Evaluation of the results of the work done.
There are three stages of dispensary:
Stage 1 - registering - includes identification of persons subject to medical examination, drawing up a plan of treatment and preventive measures and dynamic monitoring. Selection patients is carried out by a passive method when patients apply for medical help and by an active method - in the process of carrying out preventive
inspections. The first stage of dispensary is coming to an end registration medical records and drafting specific individual plan medical pro
lactic activities.
Stage 2 - performance- requires long-term follow-up. At the same time, measures are needed to improve the sanitary literacy of the population, systematic about
following patients and conducting preventive courses of treatment. In chronic tonsillitis, it is advisable to conduct such courses in spring and autumn, which corresponds to periods of exacerbation.
Stage 3 - quality and efficiency assessment dispensary observation. The results of the examination of patients and the courses of treatment carried out are reflected at the end of the year in
epicrisis. The disappearance of signs of chronic tonsillitis and exacerbations of the disease within two years are the basis for removal of the patient from the dispensary
accounting according to the compensated form of chronic tonsillitis. In the absence of the effect of the measures taken, the patient is sent for surgical treatment.
To assess the effectiveness of the organization of work, indicators of the quality of clinical examination are determined.
Acute pharyngitis is an acute inflammation of the mucous membrane of all parts of the pharynx. This disease is more often concomitant with respiratory infections of viral and microbial etiology (influenza, adenovirus, coccal).
The patient complains of a feeling of soreness or pain in the pharynx, perspiration, dryness, hoarseness, and on examination there is hyperemia of the mucosa of all parts of the pharynx, accumulation of viscous mucus on the back wall, sometimes of a hemorrhagic nature.
General symptoms - weakness, fever, discomfort - are due to the underlying disease. For the treatment of acute pharyngitis, oil-balsamic drops are recommended in the nose, a mixture in equal amounts of sea buckthorn, vaseline and menthol oils 3-5 times a day, warm alkaline inhalations, lubrication of the pharyngeal mucosa with Lugol's solution on glycerin, analgesics, aspirin are prescribed orally.
Differential diagnosis of acute pharyngitis is carried out with diphtheria, scarlet fever, measles, rubella and other infectious diseases.
Angina is an acute inflammation of the palatine tonsils and the mucous membrane of the pharynx.
Angina according to clinical data and pharyngoscopic picture is divided into catarrhal, follicular, lacunar, ulcerative-membranous and necrotic.
Angina is a common nonspecific infectious-allergic disease of predominantly streptococcal etiology, in which local inflammatory changes are most pronounced in the lymphadenoid tissue of the pharynx, most often in the palatine tonsils and regional lymph nodes.
Manifested clinically in the form of catarrhal, follicular and lacunar tonsillitis.
Nonspecific anginaNonspecific angina - catarrhal, when only the mucous membrane of the tonsils is affected, follicular - purulent damage to the follicles, lacunar - pus accumulates in the lacunae. It is usually caused by group A streptococcus.
However, there is pneumococcal tonsillitis, staphylococcal tonsillitis and tonsillitis, in the etiology of which lies a mixed coccal flora. A variety of this sore throat is alimentary sore throat, caused by epidemic streptococcus. The microbe is introduced, as a rule, in case of violation of the cooking technology by unscrupulous workers.
Catarrhal angina it affects the mucous membrane of the tonsils and arches, while hyperemia of these parts of the pharynx is noted, but there are no raids.
The patient notes pain when swallowing, burning in the pharynx. Has a bacterial or viral etiology. The temperature is subfebrile, fever is less common.
Regional lymph nodes may be moderately enlarged. The disease lasts 3-5 days. Treatment - rinsing with soda, sage, lubricating the tonsils with iodine-glycerin, ingesting aspirin.
Catarrhal angina must be distinguished from acute pharyngitis, in which the entire mucous membrane of the pharynx is affected, especially its back wall.
Follicular and lacunar tonsillitis are caused by the same pathogens and are similar in both clinical course, and by the general reaction of the body and possible complications. The difference lies in different form raids on the tonsils.
With follicular angina, suppuration of the follicles occurs, and dead white blood cells shine through the mucous membrane. With lacunar angina, inflammation begins with lacunae, where pus accumulates, then protruding from the lacunae to the surface of the tonsils.
After 1-2 days, raids spread over the entire surface of the tonsils, and it is no longer possible to distinguish between two types of tonsillitis. Patients feel severe pain when swallowing, discomfort in the throat, refuse food.
The cervical lymph nodes are sharply enlarged, the temperature rises to 39 and even 40 ° C.
On the 2nd - 3rd day, a differential diagnosis is made with diphtheria. Already at the first examination, the patient must take a smear on a diphtheria bacillus, try to remove plaque with a cotton brush.
If the plaque is removed, this speaks in favor of angina vulgaris, if it is difficult to remove, and bleeding erosion remains in its place, this is most likely diphtheria.
In case of doubt, it is necessary to introduce antidiphtheria serum.
Treatment of follicular and lacunar tonsillitis consists in rinsing the pharynx, a cervical semi-alcohol compress, prescribing analgesics, desensitizers (diphenhydramine, suprastin, tavegil), and broad-spectrum antibiotics intramuscularly. Patients are recommended a sparing diet.
Angina caused by adenoviruses, proceeds in the form of diffuse acute pharyngitis, although it may be accompanied by raids on the tonsils. Characteristic for adenovirus infection widespread lesion of the lymph nodes and a very frequent combination with conjunctivitis.
This is especially true for adenovirus type 3, which causes pharyngoconjunctival fever. A similar picture is given by the influenza virus, but in 10-12% of cases it can be combined with streptococcal tonsillitis.
Acute inflammation of the tonsils of another localization. Angina of the lingual tonsil has characteristic symptoms - pain in the deep pharynx, which increases sharply when you try to protrude the tongue.
The diagnosis is made by indirect laryngoscopy using a laryngeal mirror.
Angina of the nasopharyngeal tonsil. Pain is localized in the nasopharynx, a thick mucous discharge is released from the nose, an acute runny nose is noted. With posterior rhinoscopy, an edematous tonsil of a cyanotic color is visible, sometimes with raids, thick mucus flows down the back of the pharynx.
Angina as a syndrome of common infectious diseasesAngina with scarlet fever may proceed differently. Most often it is angina catarrhal and lacunar.
In the classic course of scarlet fever, there is a characteristic redness of the soft palate in the circumference of the pharynx, which does not extend beyond the soft palate, swelling of the cervical lymphatic glands and a whitish thick coating on the tongue, followed by its cleansing when the tongue takes on a bright color.
To make a diagnosis, it is necessary to take into account all the symptoms of the disease, especially the scarlatinal rash in the region of the mastoid process and flexor surfaces of the extremities.
Exist severe forms scarlet fever, occurring in the form of:
1) pseudomembranous angina with the formation of a fibrinous exudate widespread on the mucous membrane of the tonsils, pharynx, nasopharynx and even cheeks in the form of a thick grayish film tightly soldered to the underlying tissue. There is a bright hyperemia of the pharyngeal circumference, a rash appears already on the first day of the disease. The prognosis of this form of scarlet fever is unfavorable;
2) ulcerative necrotic angina, characterized by the appearance of grayish spots on the mucous membrane, quickly turning into ulcers. There may be deep ulceration with the formation of persistent defects of the soft palate. Lateral cervical lymph nodes are affected by extensive inflammation;
3) gangrenous tonsillitis, which is rare. The process begins with the appearance of a dirty gray plaque on the tonsils, followed by deep tissue destruction up to the carotid arteries.
Angina with diphtheria can occur in various clinical forms. With diphtheria, plaques go beyond the arches. For angina, the pathognomonic is the strict border of the distribution of raids within the tonsils. If raids spread beyond the arches, the doctor must question the diagnosis of nonspecific tonsillitis. There is a simple diagnostic test. The plaque is removed from the tonsil with a spatula and dissolved in a glass of cold water.
If the water becomes cloudy, the plaque dissolves, then it is a sore throat. If the water remains clear, and plaque particles have surfaced, then this is diphtheria.
Angina with measles proceeds under the mask of catarrh in the prodromal period and during the rash.
In the second case, the diagnosis of measles does not cause difficulties; in the prodromal period, it is necessary to monitor the appearance of measles enanthema in the form of red spots on the mucous membrane of the hard palate, as well as Filatov-Koplik spots on the inner surface of the cheeks at the opening of the stenon duct. The course of angina with measles rubella is similar to measles.
Angina with flu proceeds in the same way as catarrhal, however, diffuse hyperemia captures the tonsils, arches, tongue, back wall of the pharynx.
erysipelas is serious illness, often flowing along with the erysipelas of the face. Starts with high fever and is followed by severe pain when swallowing. The mucosa is colored bright red with sharply defined reddening borders, it seems varnished due to edema.
Angina with tularemia begins acutely - with chills, general weakness, reddening of the face, enlarged spleen.
For differential diagnosis, it is important to establish contact with rodents (water rats, house mice and gray voles) or blood-sucking insects (mosquitoes, horseflies, ticks).
Angina with tularemia in most cases occurs when infected by the alimentary route - when drinking water, food after an incubation period of 6-8 days in an infected patient.
Another differential diagnostic sign is the formation of buboes - packets of lymph nodes in the neck, sometimes reaching the size of a chicken egg.
Lymph nodes may suppurate. The picture of the pharynx may resemble catarrhal or more often membranous angina, erroneously diagnosed as diphtheria.
Angina with blood diseasesMonocytic angina(infectious mononucleosis or Filatov's disease) can clinically proceed in a variety of ways - from catarrhal to ulcerative necrotic. The etiology of this disease has not been fully elucidated. Clinically: an increase in the liver and spleen (hepatolienal syndrome), the presence of compacted and painful to the touch lymph nodes (cervical, occipital, submandibular, axillary and inguinal, and even polylymphadenitis).
A pathognomonic symptom is the appearance in the peripheral blood of atypical mononuclear cells.
Agranulocytic angina associated with the complete or almost complete disappearance of granulocytes in the peripheral blood with the preservation of monocytes and lymphocytes against the background of severe leukopenia. The etiology of the disease has not been elucidated, it is considered polyetiological. The disease is associated with excessive and uncontrolled use medicines, such as analgin, pyramidon, antipyrine, phenacytin, sulfonamides, antibiotics, chloramphenicol, Enap.
The clinical picture is usually severe and consists of symptoms of acute sepsis and necrotic tonsillitis, since the microbes that inhabit the pharynx belong to the opportunistic flora and, when the leukocyte protection is turned off and other adverse circumstances, they become pathogenic and penetrate into the tissues and blood. The disease is severe, with high fever, stomatitis, gingivitis, esophagitis. The liver is enlarged. The diagnosis is made on the basis of a blood test: severe leukopenia, below 1000 leukocytes per 1 mm 3 of blood, absence of granulocytes. The prognosis is serious due to the development of sepsis, laryngeal edema, necrosis of the tissues of the pharynx with severe bleeding. Treatment consists of fighting a secondary infection - prescribing antibiotics, vitamins, throat care (rinsing, lubricating, irrigating with antiseptic, astringent, balsamic solutions), intravenous transfusion of leukocyte mass. The prognosis for this disease is quite serious.
Alimentary-toxic aleukia characteristic in that, unlike agranulocytosis, when only granulocytes (neutrophils, eosinophils) disappear from the peripheral blood, the disappearance concerns all forms of leukocytes. The disease is associated with the ingestion of a special fungus that multiplies in overwintered cereals left unharvested in the fields and contains a very toxic substance - poin, even a very small amount of which leads to contact lesions in the form of tissue necrosis, hemorrhagic ulcers that affect the entire gastrointestinal tract, and even getting feces on the buttocks causes their ulceration.
The poison is heat-stable, so the heat treatment of flour (cooking baked goods, bread) does not reduce its toxicity.
From the side of the pharynx, necrotic sore throat is pronounced, when the tonsils look like gray dirty rags, and a sharp, nauseating smell is released from the mouth.
The number of leukocytes in the peripheral blood is up to 1000 or less, while granular leukocytes are completely absent. Characterized by high fever, the appearance of a hemorrhagic rash. Treatment at an early stage consists of gastric lavage, enemas, the appointment of a laxative, a sparing diet, intravenous infusions of saline with vitamins, hormones, glucose, blood transfusion, leukocyte mass.
In the stage of angina and necrosis, antibiotics are prescribed. With sharp clinical manifestations of the disease, the prognosis is unfavorable.
Angina in acute leukemia occur with varying degrees of severity depending on the stage of leukemia. The onset of angina (usually catarrhal) proceeds relatively favorably, begins against the background of apparent well-being, and only a blood test allows one to suspect acute leukemia at this early stage of the disease, which once again proves mandatory research blood in angina.
Angina with developed leukemia, when the number of blood leukocytes reaches 20,000 or more, and the number of erythrocytes drops to 1-2 million, angina is extremely difficult in the form of ulcerative necrotic and gangrenous forms with high fever and severe general condition. Nosebleeds, hemorrhages in organs and tissues, an increase in all lymph nodes join. The prognosis is unfavorable, patients die in 1–2 years. Treatment of angina is symptomatic, local, antibiotics and vitamins are less often prescribed.
Angina with infectious granulomas and specific pathogensTuberculosis of the pharynx can occur in two forms - acute and chronic. In the acute form, hyperemia is characteristic with a thickening of the mucous membrane of the arches, soft palate, uvula, resembling a sore throat, body temperature can reach 38 ° C and above. Observed sharp pains when swallowing, the appearance of gray tubercles on the mucous membrane, then their ulceration. A characteristic anamnesis, the presence of other forms of tuberculosis help in the diagnosis.
Of the chronic forms of tuberculosis, it is more often ulcerative, developing from infiltrations, often proceeding without symptoms. The edges of the ulcer are raised above the surface, the bottom is covered with a gray coating, after its removal, juicy granulations are found. Most often, ulcers are observed on the back of the pharynx. The course of processes in the pharynx depends on many reasons: the general condition of the patient, his nutrition, regimen, social conditions, timely and proper treatment.
In the acute miliary form of tuberculosis, the prognosis is unfavorable, the process develops very quickly with a fatal outcome in 2-3 months.
The treatment of tuberculosis of the pharynx, as well as its other forms, has become relatively successful after the advent of streptomycin, which is administered intramuscularly at 1 g per day for an average of 3 weeks. R-therapy sometimes gives good results.
Syphilis of the throat. Primary syphilis most often affects the palatine tonsils. Hard chancre is usually painless.
Usually, on a red limited background of the upper part of the tonsils, a solid infiltrate is formed, then erosion, turning into an ulcer, its surface has a cartilaginous density. There are enlarged cervical lymph nodes on the side of the lesion, painless on palpation.
Primary syphilis develops slowly, over weeks, usually on one tonsil.
The condition of patients with secondary angina worsens, fever, sharp pains appear. If syphilis is suspected, it is imperative to carry out the Wasserman reaction.
Secondary syphilis appears 2-6 months after infection in the form of erythema, papules. Erythema in the pharynx captures the soft palate, arches, tonsils, lips, surface of the cheeks, tongue. The diagnosis of syphilis at this stage is difficult until the appearance of papules from a lentil grain to a bean, their surface is covered with a touch of greasy sheen, the circumference is hyperemic.
Most often, papules are localized on the surface of the tonsils and on the arches.
The tertiary period of syphilis manifests itself in the form of gumma, which usually occurs several years after the onset of the disease. More often, gummas are formed on the back of the pharynx and soft palate. First, limited infiltration appears against the background of bright hyperemia of the pharyngeal mucosa. Complaints during this period may be absent.
With a further course, paresis of the soft palate occurs, food enters the nose. The course of tertiary syphilis is very variable, depending on the localization and rate of development of gumma, which can affect the bone walls of the facial skull, tongue, main vessels of the neck, causing profuse bleeding, grows into the middle ear.
If syphilis is suspected, a consultation with a venereologist is required to clarify the diagnosis and prescribe rational treatment.
Fusospirochetosis. The etiological factor is the symbiosis of the spindle-shaped rod and spirochete in the oral cavity. A characteristic manifestation disease is the appearance of erosions on the surface of the palatine tonsils, covered with a grayish, easily removable coating.
In the initial stage of the disease, there are no subjective sensations, the ulcer progresses, and only after 2-3 weeks there are mild pains when swallowing, regional lymph nodes on the side of the lesion may increase.
With pharyngoscopy during this period, a deep ulcer of the tonsil is found, covered with a gray fetid plaque, easily removed. General symptoms are usually not expressed.
In differential diagnosis, it is necessary to exclude diphtheria, syphilis, cancer of the tonsils, blood diseases, for which a blood test, the Wasserman reaction, and a smear for diphtheria bacillus are done.
Rarely, pharyngitis and stomatitis join the defeat of the tonsils, then the course of the disease becomes severe.
Treatment consists in the use of rinsing with hydrogen peroxide, a 10% solution of berthollet salt, potassium permanganate. However the best remedy treatment is abundant lubrication of the ulcer with a 10% solution of copper sulfate 2 times a day.
The beginning of ulcer healing is noted already on the third day, which, in turn, serves differential diagnosis with syphilis, blood diseases. The prognosis for timely treatment is favorable.
candidomycosis pharynx is caused by yeast-like fungi, often in debilitated patients or after uncontrolled intake of large doses of antibiotics that cause dysbacteriosis in the pharynx and digestive tract.
There are sore throats, fever, against the background of hyperemia of the mucous membrane of the pharynx, small white plaques appear with further extensive necrosis of the epithelium of the tonsils, arches, palate, posterior pharyngeal wall in the form of grayish plaques, after the removal of which erosion remains.
It is necessary to differentiate the disease with diphtheria, fusospirochetosis, lesions in blood diseases. The diagnosis is made on the basis of microscopy of smear materials with a coating of yeast-like fungi. Treatment involves the mandatory cancellation of all antibiotics, irrigation of the pharynx with a weak soda solution, lubrication of lesions with Lugol's solution on glycerin.
This disease must be distinguished from pharyngomycosis, in which sharp and hard spikes protruding to the surface are formed in the lacunae of the tonsils. Since there are no signs of inflammation of the surrounding tissues and subjective sensations, the disease may not be detected by the patient for a long time. Conservative treatment is ineffective. As a rule, it is necessary to remove the affected tonsils.
Peritonsillar abscessBetween the capsule of the tonsil and the pharyngeal fascia is paratonsillar fiber, and behind the pharyngeal fascia, laterally, is the fiber of the parapharyngeal space. These spaces are filled with fiber, the inflammation of which, and in the final stage - and abscessing determine the clinic of the named disease. An abscess is most often caused by nonspecific flora as a result of a tonsillogenic spread of infection. The disease begins acutely, with the appearance of pain when swallowing, often on one side.
Usually, a paratonsillar abscess occurs after suffering a sore throat during the recovery period. When examining the pharynx, there is a sharp swelling and hyperemia of the tissues around the tonsil (arches, soft palate, uvula), protrusion of the tonsil from the niche, displacement to the midline.
An abscess is formed on average about 2 days. Common symptoms are weakness, fever, enlargement of the cervical lymph nodes on the side of the abscess. The classic triad of paratonsillar abscess was noted: profuse salivation, trismus of chewing muscles and open nasality (as a result of paralysis of the muscles of the palatine curtain).
Combined treatment of abscesses is prescribed: antibiotics intramuscularly, taking into account pain when swallowing and forced starvation, aspirin, analgesics, a half-alcohol compress on the side of the neck (on the side of the abscess), antihistamines.
Simultaneously conducted surgery. There are abscesses anteroposterior (pus accumulates behind the anterior arch and soft palate near the upper pole of the tonsil), posterior (with accumulation of pus in the region of the posterior arch), external (accumulation of pus between the tonsil capsule and pharyngeal fascia). Anesthesia, as a rule, is local - lubrication of the mucous membrane with a 5% solution of cocaine or a 2% solution of dicaine. A napkin is wound around the scalpel in such a way that the tip protrudes no more than 2 mm, otherwise the main vessels of the carotid pool can be injured.
An incision is made with an anterior abscess strictly in the sagittal plane at the middle of the distance from the posterior molar to the tongue, then a blunt probe or hemostatic clamp (Holsted) is inserted into the incision and the edges of the incision are separated for better emptying of the abscess.
When the pus is removed, the patient's condition, as a rule, improves significantly. A day later, the edges of the incision are again bred with a clamp to remove the accumulated pus. In the same way, the posterior abscess is opened through the posterior arch. It is more difficult and dangerous to open an external abscess, which lies deeper and requires more caution due to the risk of injury to blood vessels. Help with this can be provided by a preliminary puncture with a syringe with a long needle, when, if pus is detected, the incision is made in the direction of the puncture. After any incision in the pharynx, furacilin is rinsed. Very rarely there is a retropharyngeal abscess - an accumulation of pus in the region of the posterior pharyngeal wall. In children, this is due to the presence of lymph nodes in the retropharyngeal space, in adults - as a continuation of the external paratonsillar abscess.
Acute inflammatory diseases of the larynx and trachea often occur as a manifestation of acute inflammatory diseases of the upper respiratory tract. The reason may be the most diverse flora - bacterial, fungal, viral, mixed.
4.4.1. Acute catarrhal laryngitis
Acute catarrhal laryngitis (laryngitis) - acute inflammationion of the mucous membrane of the larynx.
How independent disease acute catarrhal laryngitis occurs as a result of activation of the saprophytic flora in the larynx under the influence of exogenous and endogenous factors. Among exogenous factors such as hypothermia, irritation of the mucous membrane with nicotine and alcohol, exposure to occupational hazards (dust, gases, etc.), prolonged loud conversation in the cold, consumption of very cold or very hot food play a role. Endogenous factors - reduced immune reactivity, diseases of the gastrointestinal tract, allergic reactions, age-related atrophy of the mucous membrane. Acute catarrhal laryngitis often occurs during puberty when the voice mutation occurs.
Etiology. Among the various etiological factors in the occurrence of acute laryngitis, the bacterial flora plays a role - p-hemolytic streptococcus, pneumococcus, viral infections; influenza A and B viruses, parainfluenza, coronavirus, rhinovirus, fungi. Often there is a mixed flora.
Pathomorphology. Pathological changes are reduced to circulatory disorders, hyperemia, small cell infiltration and serous impregnation of the mucous membrane of the larynx. When inflammation spreads to the vestibule of the larynx, the vocal folds can be covered by edematous, infiltrated vestibular folds. When the subglottic region is involved in the process, a clinical picture of a false croup (subglottic laryngitis) occurs.
Clinic. It is characterized by the appearance of hoarseness, perspiration, a feeling of discomfort and a foreign body in the throat. Body temperature is often normal, rarely rises to subfebrile numbers. Violations of the voice-forming function are expressed in the form of varying degrees of dysphonia. Sometimes the patient is disturbed by a dry cough, which is later accompanied by expectoration of sputum.
Diagnostics. It does not present any particular difficulties, since it is based on pathognomonic signs: acute onset of hoarseness, often associated with a specific cause (cold food, SARS, colds, speech load, etc.); a characteristic laryngoscope picture - more or less pronounced hyperemia of the mucous membrane of the entire larynx or only the vocal folds, thickening, swelling and incomplete closing of the vocal folds; lack of temperature reaction if there is no respiratory infection. Acute laryngitis should also include those cases where there is only marginal hyperemia of the vocal folds, since this limited
the process, like spilled, tends to turn into chronic
In childhood, laryngitis must be differentiated from a common form of diphtheria. Pathological changes in this case will be characterized by the development of fibrinous inflammation with the formation of dirty gray films intimately associated with the underlying tissues.
Erysipelatous inflammation of the mucous membrane of the larynx differs from the catarrhal process by a clear delineation of the boundaries and simultaneous damage to the skin of the face.
Treatment. With timely and adequate treatment, the disease ends within 10-14 days, its continuation for more than 3 weeks most often indicates a transition to a chronic form. The most important and necessary therapeutic measure is the observance of the voice mode (silence mode) until the acute inflammatory phenomena subside. Failure to comply with a gentle voice regimen will not only delay recovery, but will also contribute to the transition of the process to chronic form. It is not recommended to take spicy, salty foods, alcoholic beverages, smoking, alcohol. Drug therapy mostly local. Alkaline-oil inhalations, irrigation of the mucous membrane with combined preparations containing anti-inflammatory components (Bioparox, IRS-19, etc.), infusion of medicinal mixtures of corticosteroids, antihistamines and antibiotics into the larynx for 7-10 days are effective. Effective mixtures for infusion into the larynx, consisting of 1% menthol oil, hydrocortisone emulsion with the addition of a few drops of a 0.1% solution of adrenaline hydrochloride. In the room where the patient is located, it is desirable to maintain high humidity.
For streptococcal and pneumococcal infections, accompanied by fever, intoxication, general antibiotic therapy is prescribed - penicillin preparations (phenoxymethylpenicillin 0.5 g 4-6 times a day, ampicillin 500 mg 4 times a day) or macrolides ( e.g. erythromycin 500 mg 4 times a day).
The prognosis is favorable with appropriate treatment and compliance with the voice mode.
4.4.2. Infiltrative laryngitis
Infiltrative laryngitis (laryngitis inflation) - acute inflammation of the larynx, in which the process is not limited toviscous membrane, and extends to deeper tissues. The process may involve the muscular apparatus, ligaments, supra-x.
Etiology. The etiological factor is a bacterial infection that penetrates the tissues of the larynx during injury or after an infectious disease. A decrease in local and general resistance is a predisposing factor in the etiology of infiltrative laryngitis. The inflammatory process can proceed in the form of a limited or diffuse form.
Clinic. Depends on the degree and prevalence of the process. With a diffuse form, the entire mucous membrane of the larynx is involved in the inflammatory process, with a limited one, separate parts of the larynx - the interarytenoid space, the vestibule, the epiglottis, the subvocal cavity. The patient complains of pain, aggravated by swallowing, severe dysphonia, high body temperature, feeling unwell. Possible cough with expectoration of thick mucopurulent sputum. Against the background of these symptoms, there is a violation of the respiratory function. Regional lymph nodes are dense and painful on palpation.
With irrational therapy or a highly virulent infection, acute infiltrative laryngitis can turn into a purulent form - phlegmonous laryngitis { laryngitis phlegmonosa). At the same time, pain symptoms increase sharply, body temperature rises, the general condition worsens, breathing becomes difficult, up to asphyxia. With indirect laryngoscopy, an infiltrate is detected, where a limited abscess can be seen through the thinned mucous membrane, which is a confirmation of the formation of an abscess. Abscess of the larynx may be the final stage of infiltrative laryngitis and occurs mainly on the lingual surface of the epiglottis or in the region of one of the arytenoid cartilages.
Treatment. As a rule, it is carried out in a hospital setting. Antibiotic therapy is prescribed at the maximum dosage for a given age, antihistamines, mucolytics, and, if necessary, short-term corticosteroid therapy. Emergency surgery is indicated in cases where an abscess is diagnosed. After local anesthesia, an abscess (or infiltrate) is opened with a laryngeal knife. At the same time, massive antibiotic therapy, antihistamine therapy, corticosteroid drugs, detoxification and transfusion therapy are prescribed. It is also necessary to prescribe analgesics.
Usually the process stops quickly. During the entire disease, it is necessary to carefully monitor the state of the lumen of the larynx and not wait for the moment of asphyxia.
In the presence of diffuse phlegmon with spread to the soft tissues of the neck, external incisions are made, necessarily with wide drainage of purulent cavities.
It is important to constantly monitor the function of breathing; whensigns of acute progressive stenosis require urgenttracheostomy.
4.4.3. Subglottic laryngitis (false croup)
Subglottic laryngitis -laryngitis subglottica(subchordal laryngitis- laryngitis subchordalis, false croup -false group) - acute laryngitis with predominant localization of the process insubvocal cavity. It is observed in children usually under the age of 5-8 years, which is associated with the structural features of the subglottic cavity: loose fiber under the vocal folds in young children is highly developed and easily reacts to irritation with edema. The development of stenosis is also facilitated by the narrowness of the larynx in children, the lability of nerve and vascular reflexes. With a horizontal position of the child, due to the influx of blood, the edema increases, so the deterioration is more pronounced at night.
Clinic. The disease usually begins with inflammation of the upper respiratory tract, nasal congestion and discharge, subfebrile body temperature, and cough. The general condition of the child during the day is quite satisfactory. At night, an asthma attack, barking cough, cyanosis of the skin begins suddenly. Shortness of breath is predominantly inspiratory, accompanied by retraction of the soft tissues of the jugular fossa, supraclavicular and subclavian spaces, and the epigastric region. A similar state lasts from several minutes to half an hour, after which profuse sweating appears, breathing normalizes, the child falls asleep. Similar conditions can be repeated after 2-3 days.
Laryngoscopy picture subglottic laryngitis is presented in the form of a roller-shaped symmetrical swelling, hyperemia of the mucous membrane of the subglottic space. These rollers protrude from under the vocal folds, significantly narrowing the lumen of the larynx and thereby making breathing difficult.
Diagnostics. It is necessary to differentiate from true diphtheria croup. The term "false croup" indicates that the disease is opposed to true croup, i. diphtheria of the larynx, which has similar symptoms. However, with subglottic laryngitis, the disease is paroxysmal in nature - a satisfactory condition during the day is changed by difficulty in breathing and an increase in body temperature at night. The voice with diphtheria is hoarse, with subglottic laryngitis it is not changed. With diphtheria there is no barking cough, which is characteristic of false croup. With subglottic laryngitis, there is no significant increase
cheniya regional lymph nodes, in the pharynx and larynx there are no films characteristic of diphtheria. Nevertheless, it is always necessary to conduct a bacteriological examination of smears from the pharynx, larynx and nose for diphtheria bacillus.
Treatment. It is aimed at eliminating the inflammatory process and restoring breathing. Inhalations of a mixture of decongestants are effective - 5% ephedrine solution, 0.1% adrenaline solution, 0.1% atropine solution, 1% diphenhydramine solution, 25 mg hydrocortisone and chymopsin. Antibiotic therapy is required, which is prescribed in the maximum dose for a given age, antihistamine therapy, sedatives. The appointment of hydrocortisone at the rate of 2-4 mg / kg of the child's body weight is also shown. A plentiful drink has a beneficial effect - tea, milk, mineral alkaline waters; distracting procedures - foot baths, mustard plasters.
You can try to stop the attack of suffocation by quickly touching the back of the throat with a spatula, thereby causing a gag reflex.
In the event that the above measures are powerless, andsuffocation becomes threatening, it is necessary to resort tonasotracheal intubation for 2-4 days, and if necessarytracheostomy is indicated.
4.4.4. angina
angina (angina laryngea), or submucosal laringit (laryngitis submucosa) is an acute infectious disease withdamage to the lymphadenoid tissue of the larynx, located in the ventricles of the larynx, in the thickness of the mucous membrane of the scooptan folds, at the bottom of the pear-shaped pocket, as well as in the region of the lingual surface of the epiglottis. It is relatively rare and can pass under the guise of acute laryngitis.
Etiology. The etiological factors that cause the inflammatory process are a variety of bacterial, fungal and viral flora. Penetration of the pathogen into the mucous membrane can occur by airborne or alimentary routes. Hypothermia and trauma to the larynx also play a role in etiology.
Clinic. In many ways, it is similar to the manifestations of tonsillitis of the palatine tonsils. Worried about sore throat, aggravated by swallowing and turning the neck. Possible dysphonia, difficulty breathing. Body temperature with laryngeal angina is high, up to 39 ° C, the pulse is quickened. On palpation, regional lymph nodes are painful and enlarged.
With laryngoscopy, hyperemia and infiltration of the mucous membrane of the larynx are determined, sometimes narrowing the lumen

respiratory tract, individual follicles with point purulent raids. With a prolonged course, it is possible to form an abscess on the lingual surface of the epiglottis, aryepiglottic fold and other places of accumulation of lymphadenoid tissue (Fig. 4.10).
Diagnostics. Indirect laryngoscopy with appropriate anamnestic and clinical data allows a correct diagnosis to be made. Laryngeal angina should be differentiated from diphtheria, which may have a similar course.
Treatment. Includes broad-spectrum antibiotics (augmentin, amoxiclav, cefazolin, kefzol, etc.), antihistamines (tavegil, fenkarol, peritol, claritin, etc.), mucolytics, analgesics, antipyretics. If signs of respiratory failure occur, short-term corticosteroid therapy is added to the treatment for 2-3 days. With significant stenosis, an emergency tracheotomy is indicated.
4.4.5. Laryngeal edema
Laryngeal edema (oedema laryngea) - fast-growingzomotor-allergic process in the mucous membrane of the larynx,narrowing its lumen.
Etiology. The causes of acute swelling of the larynx can be:
1) inflammatory processes of the larynx (subglottic laryngitis, acute laryngotracheobronchitis, chondroperichondritis and
acute infectious diseases (diphtheria, measles, scarlet fever, influenza, etc.);
tumors of the larynx (benign, malignant);
larynx injuries (mechanical, chemical);
allergic diseases;
pathological processes of organs adjacent to the larynx and trachea (tumors of the mediastinum, esophagus, thyroid gland, pharyngeal abscess, neck phlegmon, etc.).
Clinic. The narrowing of the lumen of the larynx and trachea can develop at lightning speed (foreign body, spasm), acute (infectious
diseases, allergic processes, etc.) and chronically (against the background of a tumor). The clinical picture depends on the degree * of the narrowing of the lumen of the larynx and the speed of its development. What would-| the faster the stenosis develops, the more dangerous it is. With inflammation! the etiology of edema is disturbed by sore throat, aggravated by! swallowing, foreign body sensation, voice change. Ras-| extension of edema to the mucous membrane of the arytenoids! cartilage, aryepiglottic folds and subglottic cavity causes acute stenosis of the larynx, causing severe! a picture of suffocation that threatens the life of the patient (see section! 4.6.1).
During laryngoscopy, swelling-1 of the mucous membrane of the affected larynx is determined in the form of! watery or gelatinous swelling. Epiglottis at! this is sharply thickened, there may be elements of hyperemia, a process! extends to the region of the arytenoid cartilages. Voice-| the gap in the mucosal edema sharply narrows, in! subglottic cavity edema looks like a bilateral pillow | bulge.
It is characteristic that with inflammatory etiology of edema on - | reactive phenomena of varying severity, hyperemia and injection of the vessels of the mucous membrane are observed. lochki, with non-inflammatory - hyperemia is usually absent - | wow.
Diagnostics. Usually no problem. Respiratory failure in varying degrees, a characteristic laryngoscopy picture allows you to correctly identify the disease.] It is more difficult to find out the cause of the edema. In some cases, hyperemic, edematous mucosa covers the tumor in the larynx, a foreign body, etc. Along with indirect laryngoscopy, it is necessary to do bronchoscopy, radiography of the larynx and chest, and other studies.
Treatment. It is carried out in a hospital and is aimed primarily at restoring external respiration. Depending on the severity of clinical manifestations, conservative and surgical methods of treatment are used.
Conservative methods are indicated for compensated and subcompensated stages of airway narrowing and include the appointment of: 1) broad-spectrum antibiotics parenterally (cephalosporins, semi-synthetic penicillins, macrolides, etc.); 2) antihistamines (2 ml pipolfen intramuscularly; tavegil, etc.); 3) corticosteroid therapy (prednisolone - up to 120 mg intramuscularly). Recommended intramuscular injection of 10 ml of 10% calcium gluconate solution, intravenously - 20 ml of 40% glucose solution simultaneously with 5 ml of ascorbic acid.
If the edema is severe and there is no positive
dynamics, the dose of administered corticosteroid drugs can be increased. A faster effect is given by intravenous administration of 200 ml of isotonic sodium chloride solution with the addition of 90 mg of prednisolone, 2 ml of pipolfen, 10 ml of 10% calcium chloride solution, 2 ml of lasix.
The lack of effect of conservative treatment, the appearance of decompensated stenosis requires immediate tracheo-stomias. With asphyxia, an emergency conicotomy is performed,
and then, after the restoration of external respiration,- tracheo-stomy.
4.4.6. Acute tracheitis
Acute tracheitis (tracheitis acuta) - acute inflammation of the mucous membrane of the lower respiratory tract (trachea and bronchi). It is rare in isolated form, in most cases acute tracheitis is combined with inflammatory changes in the upper respiratory tract - the nose, pharynx and larynx.
Etiology. The cause of acute tracheitis are infections, the pathogens of which saprophyte in the respiratory tract and are activated under the influence of various exogenous factors; viral infections, exposure to adverse climatic conditions, hypothermia, occupational hazards, etc.
Most often, when examining the discharge of the trachea, bacterial flora is detected - Staphylococcus aureus, H. in- fluenzae, Streptococcus pneumoniae, Moraxella catarrhalis and etc.
Pathomorphology. Morphological changes in the trachea are characterized by hyperemia of the mucous membrane, edema, focal or diffuse infiltration of the mucous membrane, blood filling and expansion of the blood vessels of the mucous membrane.
Clinic. Typical clinical sign with tracheitis is a paroxysmal cough, especially at night. At the beginning of the disease, the cough is dry, then mucopurulent sputum joins, sometimes with streaks of blood. After an attack of coughing, pain of varying severity behind the sternum and in the larynx is noted. The voice sometimes loses its sonority and becomes hoarse. In some cases, sub-febrile body temperature, weakness, and malaise are observed.
Diagnostics. The diagnosis is established on the basis of the results of laryngotracheoscopy, anamnesis, complaints of the patient, micro-
robiological examination of sputum, radiography of the lung.
Treatment. The patient needs to provide warm moist air in the room. Expectorants (licorice root, mukaltin, glycyram, etc.) and antitussives (libeksin, tusuprex, sinupret, broncholithin, etc.) are prescribed, mucolytic drugs (acetylcysteine, fluimucil, bromhexin), antihistamines (suprastin, pipolfen, claritin, etc.), paracetamol. The simultaneous appointment of expectorants and antitussives should be avoided. A good effect is the use of mustard plasters on the chest, foot baths.
With an increase in body temperature, in order to prevent a descending infection, antibiotic therapy is recommended (oxacillin, augmentin, amoxiclav, cefazolin, etc.).
Forecast. With rational and timely therapy, the prognosis is favorable. Recovery occurs within 2-3 weeks, but sometimes there is a protracted course and the disease can become chronic. Sometimes tracheitis is complicated by a descending infection - bronchopneumonia, pneumonia.
4.5. Chronic inflammatory diseases of the larynx
Chronic inflammatory disease of the mucous membrane and submucosa of the larynx and trachea occurs under the influence of the same causes as acute: exposure to adverse household, professional, climatic, constitutional and anatomical factors. Sometimes an inflammatory disease from the very beginning acquires a chronic course, for example, in diseases of the cardiovascular and pulmonary systems.
There are the following forms of chronic inflammation of the larynx: catarrhal, atrophic, hyperplastic; diffuseny or limited, subglottic laryngitis and pachydermialarynx.
4.5.1. Chronic catarrhal laryngitis
Chronic catarrhal laryngitis (laryngitis chronicle catar- rhalis) - chronic inflammation of the mucous membrane of the larynx. This is the most common and mildest form of chronic inflammation. The main etiological role in this pathology is played by a long-term load on the vocal apparatus (singers, lecturers, teachers, etc.). The impact is also important.
adverse exogenous factors - climatic, professional, etc.
Clinic. The most common symptom is hoarseness, a disorder of the voice-forming function of the larynx, fatigue, a change in the timbre of the voice. Depending on the severity of the disease, there is also a feeling of perspiration, dryness, sensation of a foreign body in the larynx, cough. There is a smoker's cough, which occurs against the background of prolonged smoking and is characterized by a constant, rare, mild cough.
At laryngoscopy moderate hyperemia, swelling of the mucous membrane of the larynx, more pronounced in the region of the vocal folds, against this background, a pronounced injection of the vessels of the mucous membrane are determined.
Diagnostics. It presents no difficulties and is based on a characteristic clinical picture, anamnesis and indirect laryngoscopy data.
Treatment. It is necessary to eliminate the influence of the etiological factor, it is recommended to observe a sparing voice mode (exclude loud and prolonged speech). Treatment is mostly local. During an exacerbation, an effective infusion into the larynx of a solution of antibiotics with a suspension of hydrocortisone: 4 ml of an isotonic solution of sodium chloride with the addition of 150,000 IU of penicillin, 250,000 IU of streptomycin, 30 mg of hydrocortisone. This composition is poured into the larynx 1 - 1.5 ml 2 times a day. The same composition can be used for inhalation. The course of treatment is carried out for 10 days.
With local use of drugs, antibiotics can be changed after sowing on the flora and detecting sensitivity to antibiotics. Hydrocortisone can also be excluded from the composition, and chymopsin or flu-imupil, which has a secretolytic and mucolytic effect, can be added.
Favorably, the appointment of aerosols for irrigation of the mucous membrane of the larynx with combined preparations, which include an antibiotic, analgesic, antiseptic (bioparox, IRS-19). The use of oil and alkaline oil inhalations must be limited, since these drugs have a negative effect on the ciliated epithelium, inhibiting and completely stopping its function.
A large role in the treatment of chronic catarrhal laryngitis belongs to climatotherapy in the dry sea coast.
The prognosis is relatively favorable with proper therapy, which is periodically repeated. Otherwise, a transition to a hyperplastic or atrophic form is possible.
4.5.2. Chronic hyperplastic laryngitis
Chronic hyperplastic (hypertrophic) laryngitis
(laryngitis chronicle hyperplastica) is characterized by limitedor diffuse hyperplasia of the mucous membrane of the larynx. There are the following types of hyperplasia of the mucous membrane of the larynx:
nodules of singers (singing nodules);
pachydermia of the larynx;
chronic subglottic laryngitis;
prolapse, or prolapse, of the ventricle of the larynx.
Clinic. The main complaint of the patient is persistent hoarseness of varying degrees, voice fatigue, and sometimes aphonia. During exacerbations, the patient is disturbed by perspiration, sensation of a foreign body when swallowing, a rare cough with mucous discharge.
Diagnostics. Indirect laryngoscopy and stroboscopy can detect limited or diffuse hyperplasia of the mucous membrane, the presence of thick mucus both in the intercranial and in other parts of the larynx.
In the diffuse form of the hyperplastic process, the mucous membrane is thickened, pasty, hyperemic; the edges of the vocal folds are thickened and deformed throughout, which prevents their complete closure.
With a limited form (singing nodules), the mucous membrane of the larynx Pink colour without any changes, on the border between the anterior and middle thirds of the vocal folds, there are symmetrical formations in the form of connective tissue outgrowths (nodules) on a wide base with a diameter of 1-2 mm. These nodules prevent the glottis from closing completely, resulting in a hoarse voice (Fig. 4.11).
With pachydermia of the larynx - in the interarytenoid space, the mucous membrane is thickened, on its surface there are epidermal limited outgrowths that outwardly resemble a small tuberosity, granulations are localized in the posterior third of the vocal folds and the interarytenoid space. In the lumen of the larynx there is a scant viscous discharge, in some places crusts may form.
Prolapse (prolapse) of the ventricle of the larynx occurs as a result of prolonged voice strain and inflammation of the ventricular mucosa. With forced exhalation, phonation, coughing, the hypertrophied mucous membrane protrudes from the ventricle of the larynx and partially covers the vocal folds, preventing the complete closure of the glottis, causing a hoarse voice.
Chronic subglottic laryngitis with indirect

Rice. 4.11. Limited form of hyperplastic laryngitis (singing nodules).
my laryngoscopy resembles a picture of a false croup. At the same time, there is hypertrophy of the mucous membrane of the subvocal cavity, narrowing the glottis. Anamnesis and endoscopic microlaryngoscopy allow to clarify the diagnosis.
Differential diagnosis. Limited forms of hyperplastic laryngitis must be differentiated from specific infectious granulomas, as well as from neoplasms. Appropriate serological tests and biopsy followed by histological examination help in establishing the diagnosis. Clinical experience shows that specific infiltrates do not have symmetrical localization, as in hyperplastic processes.
Treatment. It is necessary to eliminate the impact of harmful exogenous factors and obligatory observance of a sparing voice mode. During periods of exacerbation, treatment is carried out as in acute catarrhal laryngitis.
With hyperplasia of the mucous membrane, the affected areas of the larynx are quenched every other day with a 5-10% solution of silver nitrate for 2 weeks. Significant limited hyperplasia of the mucous membrane is an indication for its endolaryngeal removal with subsequent histological examination of the biopsy. The operation is performed using local application anesthesia with 10% lidocaine solution, 2% cocaine solution, 2% di- Cain. Currently, these interventions are With using endoscopic endolaryngeal methods.
4.5.3. Chronic atrophic laryngitis
Chronic atrophic laryngitis (laryngitis chronicle atro phied) characterized by degeneration of the mucous membrane of the larynx with its blanching, thinning, the formation of a viscous secretion and dry crusts.
The disease in an isolated form is rare. The cause of the development of atrophic laryngitis is most often atrophic rhinopharyngitis. Environmental conditions, occupational hazards, diseases of the gastrointestinal
tract, the absence of normal nasal breathing also contribute to the development of atrophy of the mucous membrane of the larynx.
Clinic and diagnostics. The leading complaint in atrophic laryngitis is a feeling of dryness, itching, a foreign body in the larynx, varying degrees of dysphonia. When coughing, there may be streaks of blood in the sputum due to a violation of the integrity of the epithelium of the mucous membrane at the time of the cough shock.
During laryngoscopy, the mucous membrane is thinned, smooth, shiny, sometimes covered with viscous mucus and crusts. The vocal folds are somewhat thinned. During phonation, they do not close completely, leaving an oval-shaped gap, in the lumen of which there may also be crusts.
Treatment. Rational therapy involves eliminating the cause of the disease. It is necessary to exclude smoking, the use of irritating food, a sparing voice regimen should be observed. Of the drugs, drugs are prescribed that help thin the sputum, make it easy to expectorate: irrigation of the pharynx and inhalation of an isotonic solution of sodium chloride (200 ml) with the addition of 5 drops of a 5% alcoholic solution of iodine. The procedures are carried out 2 times a day, using 30-50 ml of solution per session, in long courses for 5-6 weeks. Periodically prescribed inhalations of 1-2% menthol oil. This solution can be infused into the larynx daily for 10 days. To enhance the activity of the glandular apparatus of the mucous membrane, a 30% solution of potassium iodide is prescribed, 8 drops 3 times a day orally for 2 weeks (before the appointment, it is necessary to determine the tolerance of iodine).
With an atrophic process simultaneously in the larynx and nasopharynx, submucosal infiltration into the lateral sections of the posterior pharyngeal wall of a solution of novocaine and aloe (1 ml of a 1% solution of novocaine with the addition of 1 ml of aloe) gives a good effect. The composition is injected under the mucous membrane of the pharynx, 2 ml in each direction at the same time. Injections are repeated at intervals of 5-7 days, a total of 7-8 procedures.
4.6. Acute and chronic stenosis of the larynx and trachea
Stenosis of the larynx andtrachea expressed in the narrowing of their lumen,which prevents the passage of air into the underlyingrespiratory tract, leading to severe disorders of the externalrespiration up to asphyxia.
General phenomena in stenosis of the larynx and trachea are almost the same, therapeutic measures are also similar. Therefore, it is advisable to consider laryngeal and tracheal stenoses together. Acute or chronic stenosis of the larynx
a separate nosological unit, but a symptom complex of a disease of the upper respiratory tract and adjacent areas. This symptom complex develops rapidly, accompanied by severe impairment of the vital functions of the respiratory and cardiovascular systems, requiring emergency care. Delay in its provision can lead to the death of the patient.
4.6.1. Acute stenosis of the larynx and tracheitis
Acute laryngeal stenosis is more common than tracheal stenosis. This is due to a more complex anatomical and functional structure of the larynx, a more developed vascular network and under the mucous tissue. Acute narrowing of the airways in the larynx and trachea immediately causes severe disruption of all basic life support functions, up to their complete shutdown and death of the patient. Acute stenosis occurs suddenly or in a relatively short period of time, which, unlike chronic stenosis, does not allow the body to develop adaptive mechanisms.
The main clinical factors that are subject to immediate medical evaluation in acute laryngeal stenosis are:
the degree of insufficiency of external respiration;
the body's response to oxygen starvation.
With stenosis of the larynx and trachea, adaptornye(compensatory and protective) and pathological mechanismwe. Both are based on hypoxia and hypercapnia, which disrupt the trophism of tissues, including the brain. and nervous, which leads to excitation of the chemoreceptors of the blood vessels of the upper respiratory tract and lungs. This irritation is concentrated in the corresponding departments of the central nervous system and how the body's reserves are mobilized in response.
Adaptive mechanisms have fewer opportunities to form during the acute development of stenosis, which can lead to oppression up to complete paralysis of one or another vital function.
Adaptive responses include:
respiratory;
hemodynamic (vascular);
blood;
fabric.
Respiratory manifest as shortness of breath which leads to increase in pulmonary ventilation; in particular, going on deep-
slowing or quickening of breathing, involvement in the performance of the respiratory act of additional muscles - the back, shoulder girdle, neck.
To hemodynamic compensatory reactions include tachycardia, increased vascular tone, which increases the minute volume of blood by 4-5 times, accelerates blood flow, increases blood pressure, and removes blood from the depot. All this enhances the nutrition of the brain and vital organs, thereby reducing oxygen deficiency, improves the removal of toxins that have arisen in connection with stenosis of the larynx.
Bloody and tissue adaptive reactions are the mobilization of erythrocytes from the spleen, an increase in vascular permeability and the ability of hemoglobin to be completely saturated with oxygen, and an increase in erythropoiesis. The ability of the tissue to absorb oxygen from the blood increases, a partial transition to an anaerobic type of metabolism in cells is noted.
All these mechanisms can, to a certain extent, reduce hypoxemia (lack of oxygen in the blood), hypoxia (in tissues), as well as hypercapnia (increase in CO 2 content in the blood). Insufficiency of pulmonary ventilation can be compensated for if a minimum volume of air enters the lung, which is individual for each patient. The increase in stenosis, and consequently, hypoxia under these conditions, leads to the progression of pathological reactions, the mechanical function of the left ventricle of the heart is disturbed, hypertension appears in the small circle, the respiratory center is depleted, and gas exchange is sharply disturbed. Metabolic acidosis occurs, the partial pressure of oxygen falls, oxidative processes decrease, hypoxia and hypercapnia are not compensated.
Etiology. The etiological factors of acute stenosis of the larynx and trachea can be endogenous and exogenous. Among the first local inflammatory diseases - swelling of the larynx and trachea, subglottic laryngitis, acute laryngotracheobron-hit, larynx chondroperichondritis, laryngeal tonsillitis. Non-inflammatory processes - tumors, allergic reactions, etc. General diseases of the body - acute infectious diseases (measles, diphtheria, scarlet fever), diseases of the heart, blood vessels, kidneys, endocrine diseases. Among the latter, the most common are foreign bodies, injuries of the larynx and trachea, the condition after bronchoscopy, and intubation.
Clinic. The main symptom of acute stenosis of the larynx and trachea is shortness of breath, noisy, intense breathing. Depending on the degree of narrowing of the airways, on examination, retraction of the supraclavicular fossae, retraction of the intercostal spaces, and a violation of the rhythm of breathing are observed. These signs are associated with an increase in negative pressure in the mediastinum during inspiration. It should be noted that with stenosis on
at the level of the larynx, shortness of breath is inspiratory in nature, the voice is usually changed, and with narrowing of the trachea, expiratory shortness of breath is observed, the voice is not changed. A patient with severe stenosis develops a feeling of fear, motor excitation (he rushes about, tends to run), face flushing, sweating, cardiac activity, secretory and motor function of the gastrointestinal tract, urinary function of the kidneys are disturbed. If the stenosis continues, there is an increase in the pulse, cyanosis of the lips, nose and nails. This is due to the accumulation of CO 2 in the body. There are 4 stages of airway stenosis:
I - stage of compensation; II - stage of subcompensation;
Stage of decompensation;
Stage of asphyxia (terminal stage).
In the compensation stage, due to a decrease in oxygen tension in the blood, the activity of the respiratory center increases, and at the same time, an increase in the content of CO 2 in the blood can directly irritate the cells of the respiratory center, which is manifested by a decrease and deepening of respiratory excursions, a shortening or loss of pauses between inhalation and exhalation, a decrease in number of pulse beats. The width of the glottis is 6-7 mm. At rest there is no lack of breath, while walking and physical activity shortness of breath appears.
In the stage of subcompensation, the phenomena of hypoxia deepen, and the respiratory center becomes weaker. Already at rest, inspiratory dyspnea appears (difficulty inhaling) with the inclusion of auxiliary muscles in the act of breathing. At the same time, retraction of the intercostal spaces, soft tissues of the jugular, supraclavicular and subclavian fossae, swelling (fluttering) of the wings of the nose, stridor (breathing noise), pallor of the skin, restless state of the patient are noted. The width of the glottis is 4-5 mm.
In the stage of decompensation, the stridor is even more pronounced, the tension of the respiratory muscles becomes maximum. Breathing is frequent and superficial, the patient takes a forced semi-sitting position, tries to hold on to the headboard or other object with his hands. The larynx makes maximum excursions. The face acquires a pale bluish color, a feeling of fear appears, cold sticky sweat, cyanosis of the lips, tip of the nose, distal (nail) phalanges, the pulse becomes frequent. The width of the glottis is 2-3 mm.
In the stage of asphyxia with acute stenosis of the larynx, breathing is intermittent, according to the Cheyne-Stokes type, gradually the pauses between the respiratory cycles increase and stop altogether. The width of the glottis is 1 mm. There is a sharp drop in cardiac activity, the pulse is frequent, thready,
blood pressure is not determined, the skin is pale gray due to spasm of small arteries, the pupils dilate. In severe cases, loss of consciousness, exophthalmos, involuntary urination, defecation are observed. and death comes quickly.
Diagnostics. It is based on the described symptoms, data of indirect laryngoscopy, tracheobronchoscopy. It is necessary to find out the causes and location of the narrowing. There are a number of clinical features to distinguish between laryngeal and tracheal stenosis. With laryngeal stenosis, it is mainly difficult to inhale, i.e. shortness of breath is inspiratory in nature, and with tracheal - exhalation (expiratory type of shortness of breath). The presence of an obstruction in the larynx causes hoarseness, while the constriction in the trachea leaves the voice clear. Differentiate acute stenosis from laryngospasm, bronchial asthma, uremia.
Treatment. It is carried out depending on the cause and stage of acute stenosis. With compensated and subcompensated stages, it is possible to use drug treatment in a hospital setting. For laryngeal edema, dehydration therapy, antihistamines, and corticosteroids are used. In inflammatory processes in the larynx, massive antibiotic therapy, anti-inflammatory drugs are prescribed. In diphtheria, for example, it is necessary to administer a specific anti-diphtheria serum.
The most efficient way to medical destination, the scheme of which is set out in the relevant sections on the treatment of laryngeal edema.
With decompensated stage of stenosis urgent need tracheostomy, and in the stage of asphyxia, a conicotomy is urgently performed, and then a tracheostomy.
It should be noted that with appropriate indicationsthe doctor is obliged to perform these operations in almost anyconditions and without delay.
In relation to the isthmus thyroid gland depending on the level of the incision are distinguished upper tracheostomy -above the isthmus of the thyroid gland (Fig. 4.12), lower under itand middle through the isthmus, with its preliminary dissection anddressing. It should be noted that this division is conditional due tovarious options for the location of the isthmus of the thyroid gland in relation to the trachea. More acceptable is the division depending on the level of the incision of the tracheal rings. At the toptracheostomy cut 2-3 rings, with an average of 3-4 rings andat the bottom 4-5 rings.
The technique of upper tracheostomy is as follows. The position of the patient is usually recumbent, it is necessary to put a roller under the shoulders to protrude the larynx and facilitate orientation.

Rice. 4.12. Tracheostomy.
a - median incision of the skin and dilution of the edges of the wound; b - exposure of the rings
trachea; c - dissection of the tracheal rings.
Sometimes, with rapidly developing asphyxia, an operation is performed in a semi-sitting or sitting position. Local anesthesia - 1% novocaine solution mixed with 0.1% adrenaline solution (1 drop per 5 ml). The hyoid bone, the lower notch of the thyroid and the arch of the cricoid cartilage are palpated. For orientation, you can brilliant green from-

Rice. 4.12. Continuation.
d - formation of a tracheostomy.
mark the midline and the level of the cricoid cartilage. A layer-by-layer incision of the skin and subcutaneous tissue is made from the lower edge of the thyroid cartilage by 4-6 cm, vertically downwards strictly along the midline. The superficial plate of the cervical fascia is dissected, under which a white line is found - the junction of the sternohyoid muscles. The latter is incised and the muscles are gently cut off in a blunt way. After that, a part of the cricoid cartilage and the isthmus of the thyroid gland are observed, which has a dark red color and is soft to the touch. Then an incision is made in the capsule of the gland that fixes the isthmus, the latter is displaced downwards and held with a blunt hook. After that, the tracheal rings covered with fascia become visible. Careful hemostasis is necessary to open the trachea. To fix the larynx, the excursions of which are significantly pronounced during asphyxia, a sharp hook is injected into the thyroid-hyoid membrane. To avoid severe cough a few drops of a 2-3% dicaine solution are injected into the trachea. With a pointed scalpel, 2-3 tracheal rings are opened. The scalpel must not be inserted too deeply so as not to injure the posterior, cartilage-free wall of the trachea and the anterior wall of the esophagus adjacent to it. The size of the incision should correspond to the size of the tracheotomy tube. To form a tracheostomy, the skin around the wound on the neck is separated from the underlying tissues and sutured to the perichondrium of the dissected tracheal rings with four silk threads. The edges of the tracheostomy are moved apart with a Trousseau dilator and a tracheotomy tube is inserted. The latter is fixed with a gauze bandage around the neck.
In some cases, in pediatric practice, with stenosis caused by diphtheria of the larynx and trachea, naso(oro) is used.
tracheal intubation with a flexible synthetic tube. Intubation is performed under the control of direct laryngoscopy, its duration should not exceed 3 days. If a longer period of intubation is needed, a tracheostomy is performed, since a long stay of the endotracheal tube in the larynx causes ischemia of the mucous membrane of the wall, followed by its ulceration, scarring and persistent stenosis of the organ.
4.6.2. Chronic stenosis of the larynx and trachea
Chronic stenosis of the larynx and trachea- prolonged and irreversible narrowing of the airway lumen, causing a number of severe complications from other organs and systems. Persistent morphological changes in the larynx and trachea or in adjacent areas usually develop slowly over a long period of time.
The causes of chronic stenosis of the larynx and trachea are varied. The most frequent are:
surgical interventions and injuries during laryngotracheal operations, prolonged tracheal intubation (over 5 days);
benign and malignant tumors larynx and trachea;
traumatic laryngitis, chondroperichondritis;
thermal and chemical burns larynx;
prolonged stay of a foreign body in the larynx and trachea;
impaired function of the lower laryngeal nerves as a result of toxic neuritis, after strumectomy, with compression by a tumor, etc.;
congenital malformations, cicatricial membranes of the larynx;
specific diseases of the upper respiratory tract (tuberculosis, scleroma, syphilis, etc.).
Often in practice, the development of chronic stenosis of the larynx is due to the fact that tracheostomy is performed with a gross violation of the operation technique: instead of the second or third tracheal ring, the first is cut. In this case, the tracheotomy tube touches the lower edge of the cricoid cartilage, which always quickly causes chondroperichondritis, followed by severe stenosis of the larynx.
Prolonged wearing of a tracheotomy tube and its incorrect selection can also cause chronic stenosis.
Clinic. Depends on the degree of narrowing of the airways and the cause of the stenosis. However, the slow and gradual increase in stenosis gives time for the development of adaptive mechanisms of the body, which allows even under conditions
insufficiency of external respiration to maintain life support functions. Chronic stenosis of the larynx and trachea has a negative effect on the entire body, especially in children, which is associated with oxygen deficiency and a change in reflex influences emanating from receptors located in the upper respiratory tract. Violation of external respiration leads to sputum retention and frequent recurrent bronchitis and pneumonia, which ultimately leads to the development of chronic pneumonia with bronchiectasis. With a long course of chronic stenosis, these complications are accompanied by changes in the cardiovascular system.
Diagnostics. Based on characteristic complaints, anamnesis. The study of the larynx to determine the nature and localization of stenosis is performed by indirect and direct laryngoscopy. Diagnostic capabilities have expanded significantly in recent years due to the use of bronchoscopy and endoscopic methods that allow you to determine the level of the lesion, its prevalence, scar thickness, appearance pathological process, the width of the glottis.
Treatment. Small cicatricial changes that do not interfere with breathing do not require special treatment. Cicatricial changes that cause persistent stenosis require appropriate treatment.
For certain indications, expansion (bougienage) of the larynx is sometimes used with bougies growing in diameter and special dilators for 5-7 months. With a tendency to narrowing and ineffectiveness of long-term dilatation, the airway lumen is restored surgically. Operative plastic interventions on the upper respiratory tract are usually performed by an open method and represent various variants of laryngopharyngotracheofissure. These surgical interventions are difficult to perform and are multi-stage in nature.
4.7. Diseases of the nervous apparatus of the larynx
Among the diseases of the nervous apparatus of the larynx, there are:
sensitive;
movement disorders.
Depending on the localization of the main process, disorders of the innervation of the larynx can be of central or peripheral origin, and by nature - functional or organic.
4.7.1. Sensitivity disorders
Disorders of the sensitivity of the larynx can be caused by central (cortical) and peripheral causes. Central disorders, usually caused by a violation of the ratio of the processes of excitation and inhibition in the cerebral cortex, are bilateral in nature. At the heart of naru-; Neuropsychiatric diseases (hysteria, neurasthenia, functional neuroses, etc.) lie at the root of the sensitive innervation of the larynx. Hysteria, according to I.P. Pavlov, is the result of a breakdown of higher nervous activity in people with insufficient coordination of work signaling systems, expressed in the predominance of the activity of the first signal system and the subcortex over the activity of the second signal system. In easily suggestible persons, a violation of the function of the larynx, which has arisen under the influence of a nervous shock, fright, can be fixed, and these disorders take on a long-term character. Sensitivity disorder manifests itself hypoesthesia(decrease in sensitivity) of varying severity, up to anesthesia, or hyperesthesia(increased sensitivity) and paresthesia(perverted sensibility).
hypoesthesia or anesthesia larynx is more often observed with traumatic injuries of the larynx or superior laryngeal nerve, with surgical interventions on the organs of the neck, with diphtheria, with anaerobic infection. A decrease in the sensitivity of the larynx usually causes minor subjective sensations in the form of tickling, awkwardness in the throat, and dysphonia. However, against the background of a decrease in the sensitivity of the reflexogenic zones of the larynx, there is a danger of pieces of food and liquid getting into the respiratory tract and, as a result, the development of aspiration pneumonia, impaired external respiration, up to asphyxia.
Hyperesthesia can be of varying severity and is accompanied by a painful sensation when breathing and talking, often there is a need to expectorate mucus. With hyperesthesia, it is difficult to examine the oropharynx and larynx due to a pronounced gag reflex.
paresthesia it is expressed by a wide variety of sensations in the form of tingling, burning, sensation of a foreign body in the larynx, spasm, etc.
Diagnostics. It is based on the data of the anamnesis, the patient's complaints and the laryngoscopy picture. In diagnosis, it is possible to apply the method of assessing the sensitivity of the larynx during probing: touching the mucous membrane of the wall of the larynx with a cotton probe causes an appropriate response. Along with this, it is necessary to consult a neuropathologist, a psychotherapist.
Treatment. It is carried out together with a neurologist. By-
Since disorders of the central nervous system lie at the heart of sensitivity disorders, therapeutic measures are aimed at their elimination. Assign sedative therapy, coniferous baths, vitamin therapy, spa treatment. In some cases, novocaine blockades are effective, both in the area ganglions, and along the pathways. Of the physiotherapeutic agents for peripheral lesions, intra- and extralaryngeal galvanization, acupuncture, homeopathic remedies are prescribed.
4.7.2. Movement disorders
Movement disorders of the larynx are manifested in the form of partial (paresis) or complete (paralysis) loss of its functions. Such disorders can result from an inflammatory and regenerative process in both the muscles of the larynx and the laryngeal nerves. They can be central and peripheral origin. Distinguish myogenic and neuro-gene paresis and paralysis.
♦ Central paralysis of the larynx
Paralysis of central (cortical) origin develops with craniocerebral trauma, intracranial hemorrhage, multiple sclerosis, syphilis, etc.; may be unilateral or bilateral. Paralysis of central origin is more often associated with damage to the medulla oblongata and is combined with paralysis of the soft palate.
Clinic. It is characterized by speech disorders, sometimes respiratory failure and convulsions. Motor disorders of central origin often develop in the last stage of severe brain disorders, which are difficult to cure.
Diagnostics. Based on characteristic symptoms underlying disease. With indirect laryngoscopy, there is a violation of the mobility of one or both halves of the larynx.
Treatment. Aimed at eliminating the underlying disease. Local disorders in the form of difficulty in breathing sometimes require surgical intervention (tracheostomy is performed). In some cases, it is possible to use physiotherapy in the form of electrophoresis of drugs and electrical stimulation of the muscles of the larynx. Favorable effect has climatic and phonopedic treatment.
♦ Peripheral paralysis of the larynx
Peripheral paralysis of the larynx, as a rule, is unilateral and is caused by a violation of the innervation of the muscles by the laryngeal, mainly recurrent, nerves, which is explained
the topography of these nerves, the proximity to many organs of the neck and chest cavity, diseases of which can cause dysfunction of the nerve.
Paralysis of the muscles innervated by the recurrent laryngeal nerves is most often caused by tumors of the esophagus or mediastinum, enlarged parabronchial and mediastinal lymph nodes, syphilis, cicatricial changes in the apex of the lung. The causes of damage to the recurrent nerve can also be an aneurysm of the aortic arch for the left nerve and an aneurysm of the right subclavian artery for the right recurrent laryngeal nerve, as well as surgical interventions. The left recurrent laryngeal nerve is most commonly affected. With diphtheria neuritis, paralysis of the larynx is accompanied by paralysis of the soft palate.
Clinic. Hoarseness and weakness of the voice of varying severity are characteristic functional symptoms of paralysis of the larynx. With bilateral damage to the recurrent laryngeal nerves, there is a violation of breathing, while the voice remains sonorous. In childhood, choking occurs after eating, associated with the loss of the protective reflex of the larynx.
With laryngoscopy, characteristic mobility disorders of the arytenoid cartilages and vocal folds are determined, depending on the degree of movement disorders. In the initial stage of unilateral paresis of the muscles innervated by the recurrent laryngeal nerve, the vocal fold is somewhat shortened, but retains limited mobility, moving away from the midline during inspiration. In the next stage, the vocal fold on the side of the lesion becomes motionless and is fixed in the middle position, occupies the so-called cadaveric position. Subsequently, compensation appears from the side of the opposite vocal fold, which goes beyond the midline and approaches the vocal fold of the opposite side, which retains a sonorous voice with a slight hoarseness.
Diagnostics. In violation of the innervation of the larynx, it is necessary to identify the cause of the disease. X-ray examination and computed tomography of the chest organs are performed. To exclude syphilitic neuritis, it is necessary to examine the blood according to Wasserman. Vocal cord paralysis, accompanied by spontaneous rotatory nystagmus on one side, indicates damage to the nuclei of the medulla oblongata.
Treatment. With motor paralysis of the larynx, the underlying disease is treated first. With paralysis of inflammatory etiology, anti-inflammatory therapy, physiotherapy procedures are carried out. With toxic neuritis, for example, with syphilis, special
physical therapy. Persistent laryngeal mobility disorders caused by tumors or cicatricial processes are treated promptly. Plastic surgeries are effective - removal of one vocal fold, excision of the vocal folds, etc.
♦ Myopathic paralysis
Myopathic paralysis is caused by damage to the muscles of the larynx. In this case, the constrictors of the larynx are predominantly affected. The most common is vocal paralysis. With bilateral paralysis of these muscles during phonation, an oval-shaped gap is formed between the folds (Fig. 4.13, a). Paralysis of the transverse arytenoid muscle laryngoscopy is characterized by the formation of a triangular space in the posterior third of the glottis due to the fact that with paralysis of this muscle, the bodies of the arytenoid cartilages do not approach completely along the midline (Fig. 4.13, b). The defeat of the lateral cricoarytenoid muscles leads to the fact that the glottis acquires the shape of a rhombus.
Diagnostics. Based on history and laryngoscopy.
Treatment. It is aimed at eliminating the cause that caused paralysis of the laryngeal muscles. Locally used physiotherapy procedures (electrotherapy), acupuncture, food and voice mode. To increase the tone of the muscles of the larynx, faradization and vibromassage have an effect. A good effect is produced by phonopedic treatment, in which, with the help of special sound and breathing exercises, the speech and respiratory functions of the larynx are restored or improved.

Rice. 4.13. Motor disorders of the larynx.
laryngospasm
Convulsive narrowing of the glottis, which involves almost all the muscles of the larynx - laryngospasm, occurs more often in childhood. The cause of laryngospasm is hypocalcemia, lack of vitamin D, while the calcium content in the blood decreases to 1.4-1.7 mmol/l instead of the normal 2.4-2.8 mmol/l. Laryngospasm may be hysteroid.
Clinic. Laryngospasm usually occurs suddenly after a strong cough, fright. Initially, there is a noisy, uneven long breath, followed by intermittent shallow breathing. The child's head is thrown back, the eyes are wide open, the neck muscles are tense, the skin is cyanotic. There may be cramps in the limbs, facial muscles. After 10-20 seconds, the respiratory reflex is restored. In rare cases, the attack ends in death due to cardiac arrest. Due to increased muscle excitability, the production of surgical interventions - adenotomy, opening of the pharyngeal abscess, etc., in such children is associated with dangerous complications.
Diagnostics. Spasm of the glottis is recognized on the basis of the clinic of the attack and the absence of any changes in the larynx in the interictal period. At the time of the attack, with direct laryngoscopy, one can see a folded epiglottis, the aryepiglottic folds converge along the midline, the arytenoid cartilages are brought together and everted.
Treatment. Laryngospasm can be eliminated by any strong stimulus of the trigeminal nerve - an injection, a pinch, pressure on the root of the tongue with a spatula, spraying the face cold water and others. With prolonged spasm, intravenous administration of a 0.5% solution of novocaine is favorable.
In threatening cases, a tracheotomy or conicotomy should be resorted to.
In the post-attack period, general strengthening therapy, calcium preparations, vitamin D, and fresh air are prescribed. With age (usually by 5 years), these phenomena are eliminated.
4.8. Injuries of the larynx and trachea
Injuries of the larynx and trachea, depending on the damaging factor, can be mechanical, thermal, radiation and chemical. There are also open and closed injuries.
In peacetime, injuries to the larynx and trachea are relatively rare.
♦ Open injuries
Open injuries, or wounds, of the larynx and tracheas, as a rule, are combined in nature, with them not only the larynx itself is damaged, but also the organs of the neck, face, and chest. There are cut, stab and gunshot wounds. Incised wounds occur as a result of damage caused by various cutting tools. Most often they are applied with a knife or razor for the purpose of murder or suicide (suicide). According to the level of the location of the incision, there are: 1) wounds located under the hyoid bone, when the thyroid-hyoid membrane is cut; 2) injuries of the subvocal area. In the first case, due to the contraction of the cut muscles of the neck, the wound, as a rule, gapes widely, due to which it is possible to examine the larynx and part of the pharynx through it. The epiglottis with such wounds always goes up, breathing and voice are preserved, but speech is absent with a gaping wound, since the larynx is separated from the articulatory apparatus. If in this case the edges of the wound are moved, thereby closing its lumen, then speech is restored. When food is swallowed, it comes out through the wound.
Clinic. The general condition of the patient is significantly disturbed. Blood pressure drops, pulse quickens, body temperature rises. When the thyroid gland is injured, significant bleeding occurs. Consciousness, depending on the degree and nature of the injury, can be preserved or confused. If the carotid arteries are injured, death occurs immediately. However, carotid arteries are rarely crossed in suicidal wounds; suicides throw their heads back strongly, sticking out their neck, while the arteries are displaced backwards.
Diagnostics presents no difficulty. It is necessary to determine the level of the location of the wound. Seeing through the wound and probing allows you to determine the state of the cartilaginous skeleton of the larynx, the presence of edema, hemorrhage.
Treatment surgical, includes stopping bleeding, ensuring adequate breathing, replenishing blood loss and primary wound treatment. Particular attention should be paid to the respiratory function. As a rule, a tracheostomy is performed, preferably lower.
If the wound is located in the region of the thyroid-hyoid membrane, the wound should be sutured in layers with the obligatory suturing of the larynx to the hyoid bone with chrome-plated catgut. Before suturing the wound, it is necessary to stop the bleeding in the most thorough way by bandaging or suturing the vessels. To reduce tension and provide
convergence of the edges of the wound, the patient's head is tilted forward during suturing. If necessary, for a complete revision, the wound should be widely incised. If the mucous membrane of the larynx is damaged, its possible suturing is performed, the formation of a laryngostomy and the introduction of a T-shaped tube. In order to protect against infection, the patient is fed with a gastric tube inserted through the nose or mouth. At the same time, anti-inflammatory and restorative treatment is prescribed, including the introduction of massive doses of antibiotics, antihistamines, detoxification drugs, hemostatics, and anti-shock therapy.
■ Gunshot wounds of the larynx and trachea. These injuries are rarely isolated. More often they are combined with damage to the pharynx, esophagus, thyroid gland, vessels and nerves of the neck, spine, spinal cord and brain.
Gunshot wounds of the larynx and trachea are divided into through,blindandtangents (tangential).
With a through wound, as a rule, there are two holes - inlet and outlet. It must be taken into account that the inlet rarely coincides with the course of the wound channel, the site of damage to the larynx and the outlet, since the skin and tissues on the neck are easily displaced.
With blind wounds, a fragment or a bullet gets stuck in the larynx or in soft tissues neck. Once in the hollow organs - the larynx, trachea, esophagus, they can be swallowed, spit out or aspirated into the bronchus.
With tangential (tangential) wounds, the soft tissues of the neck are affected without violating the integrity of the mucous membrane of the larynx, trachea, and esophagus.
Clinic. Depends on the depth, degree, type and translational force of the wounding projectile. The severity of the wound may not correspond to the size and strength of the injuring projectile, since the concomitant contusion of the organ, violation of the integrity of the skeleton, hematoma and swelling of the internal lining aggravate the patient's condition.
The wounded is often unconscious, shock is often observed, as the vagus nerve is injured and sympathetic trunk and, in addition, when large vessels are injured, large blood loss occurs. An almost constant symptom is difficulty in breathing due to injury. and compression of the airways by edema and hematoma. Emphysema occurs when the wound opening is not large sizes and slips quickly. Swallowing is always disturbed and accompanied by severe pain; food, getting into the respiratory tract, contributes to the occurrence of cough and the development of an inflammatory complication in the lung.
,...■,.■■■. ■ . ■■■ ■ . ■ 309
Diagnostics. Based on history and physical examination. The cervical wound is mostly wide, with torn edges, with significant loss of tissue and the presence of foreign bodies - metal fragments, pieces of tissue, particles of gunpowder in the wound, etc. When wounded at close range, the edges of the wound are burned, there is hemorrhage around it. In some wounded, soft tissue emphysema is determined, which indicates the penetration of the wound into the cavity of the larynx or trachea. This may also indicate hemoptysis.
Laryngoscopy (direct and indirect) in the wounded is often practically impossible due to severe pain, inability to open the mouth, fractures of the jaw, hyoid bone, etc. In the following days, with laryngoscopy, it is necessary to determine the condition of the region of the vestibule of the larynx, glottis and subglottic cavity. Hematomas, ruptures of the mucous membrane, damage to the cartilage of the larynx, the width of the glottis are revealed.
Informative in the diagnosis of the x-ray method of research, computed tomography data, with which you can determine the state of the skeleton of the larynx, trachea, the presence and localization of foreign bodies.
Treatment. In case of gunshot wounds, it includes two groups of measures: 1) restoration of breathing, stopping bleeding, primary treatment of the wound, combating shock; 2) anti-inflammatory, desensitizing, restorative therapy, anti-tetanus (possibly others) vaccination.
To restore breathing and prevent further impairment of respiratory function, as a rule, a tracheotomy is performed with the formation of a tracheostomy.
Bleeding is stopped by applying ligatures to the vessels in the wound, and if large vessels are damaged, the external carotid artery is ligated.
The fight against pain shock includes the introduction of narcotic analgesics, transfusion therapy, single-group blood transfusion, and cardiac drugs.
Primary surgical treatment of the wound, in addition to stopping bleeding, includes gentle excision of crushed soft tissues, removal of foreign bodies. With extensive damage to the larynx, a laryngostomy should be formed with the introduction of a T-shaped tube. After emergency measures, it is necessary to introduce anti-tetanus serum according to the scheme (if serum was not administered earlier before the operation).
The second group of measures includes the appointment of broad-spectrum antibiotics, antihistamines, dehydration and corticosteroid therapy. Patients are fed through a nasoesophageal tube. When introducing the probe, one should be careful not to get it into the respiratory tract, which is determined by the occurrence of a cough, difficulty breathing. "■>
♦ Closed injuries
Closed injuries of the larynx and trachea occur when various foreign bodies, metal objects, etc. get into the cavity of the larynx and the subvocal cavity or with a blunt blow from the outside, falling on the larynx. Often, the mucous membrane of the larynx is injured by a laryngoscope or endotracheal tube during anesthesia. An abrasion, hemorrhage, and a violation of the integrity of the mucous membrane are found at the site of injury. Sometimes swelling appears at the site of injury and around it, which can spread, and then it poses a threat to life. If an infection enters the site of injury, a purulent infiltrate may appear, the possibility of developing phlegmon and chondroperi-chondritis of the larynx is not excluded.
With prolonged or rough exposure of the endotracheal tube to the mucous membrane, in some cases a so-called intubation granuloma is formed. The most common location for it is the free edge of the vocal fold, since in this place the tube is most closely in contact with the mucous membrane.
Clinic. With a closed injury of the mucous membrane of the larynx and trachea by a foreign body, a sharp pain occurs, which is aggravated by swallowing. Edema and tissue infiltration develop around the wound, which can lead to breathing difficulties. Due to sharp pain, the patient cannot swallow saliva, eat food. The accession of a secondary infection is characterized by the appearance of pain on palpation of the neck, increased pain when swallowing, and an increase in body temperature.
With external blunt trauma, swelling of the soft tissues of the larynx on the outside and swelling of the mucous membrane, more often in its vestibular region, are noted.
Diagnostics. Based on anamnesis data and objective research methods. Laryngoscopy may show swelling, hematoma, infiltrate, or abscess at the site of injury. In the pear-shaped pocket or in the pits of the epiglottis on the side of the lesion, saliva may accumulate in the form of a lake. Radiography in direct and lateral projections, as well as with the use of contrast agents, in some cases makes it possible to detect a foreign body, to determine the level of a possible fracture of the cartilage of the larynx.
Treatment. The tactics of managing the patient depends on the patient's examination data, the nature and area of damage to the mucous membrane, the state of the airway lumen, the width of the glottis, etc. If there is an abscess, it is necessary to open it with a laryngeal (hidden) scalpel after preliminary application anesthesia. When expressed
respiratory disorders (stenosis II- III degree) requires an emergency tracheostomy.
In edematous forms, to eliminate stenosis, drug destenosis is prescribed (corticosteroid, antihistamine, dehydration drugs).
In all cases of closed injuries of the larynx occurring against the background of a secondary infection, antibiotic therapy, antihistamines and detoxification agents are necessary.
Everyone in life had to meet with various diseases ENT organs, most often viral or bacterial infections in the form of SARS, flu or tonsillitis. But there are a number of other pathologies, the symptoms of which you need to know in order to diagnose the disease in time.
The structure of the pharynx and larynx
To understand the essence of diseases, you should have a minimal understanding of the structure of the larynx and pharynx.
Regarding the pharynx, it consists of three sections:
- upper, nasopharynx;
- oropharynx, middle section;
- laryngopharynx, lower section.
The larynx is an organ that performs several functions. The larynx is the conductor of food to the digestive tube, it is also responsible for the flow of air into the trachea and lungs. In addition, the vocal cords are located in the larynx, thanks to which a person has the ability to make sounds.
The larynx functions as a movement apparatus that has cartilage connected to the ligaments and joints of the muscles. At the beginning of the organ is the epiglottis, the function of which is to create a valve between the trachea and the pharynx. At the moment of swallowing food, the epiglottis blocks the entrance to the trachea, so that food enters the esophagus, and not into the respiratory system.
What are the pathologies of ENT organs
According to their course, diseases are classified into: chronic and acute. In the case of an acute course of the disease, the symptoms develop instantly, they are pronounced. Pathology is more difficult to tolerate than with chronic course, but recovery comes faster, on average in 7-10 days.
Chronic pathologies occur against the background of a constant, untreated inflammatory process. In other words, the acute form becomes chronic without proper treatment. In this case, the symptoms do not appear so rapidly, the process is sluggish, but complete recovery does not occur. At the slightest provoking factors, for example, hypothermia or a virus entering the body, a relapse occurs chronic disease. As a result of a constant infectious focus, human immunity is weakened, because of this, it is not difficult for a virus or bacteria to penetrate.
Diseases of the pharynx and larynx:
- epiglottitis;
- pharyngitis;
- tonsillitis;
- laryngitis;
- nasopharyngitis;
- adenoids;
- throat cancer.
Epiglottitis
Diseases of the larynx include inflammation of the epiglottis (epiglottitis). The cause of the inflammatory process is the entry of bacteria into the epiglottis by airborne droplets. Most often, the epiglottis affects hemophilus influenzae and becomes the cause of the inflammatory process. The bacterium can not only cause disease of the epiglottis, but is also the causative agent of meningitis, pneumonia, pyelonephritis and other pathologies. In addition to hemophilus influenza, inflammation of the epiglottis can cause:
- streptococci;
- pneumococci;
- fungus candida;
- burn or foreign body in the epiglottis.
Symptoms of the disease develop rapidly, among the main ones are: 
- complicated breathing with wheezing. In the epiglottis, edema occurs, which leads to a partial overlap of the larynx and trachea, which complicates the possibility of normal air intake;
- pain when swallowing, difficulty in swallowing food with a feeling that something is in the larynx, something is in the way;
- throat redness, pain in him;
- fever and fever;
- general weakness, malaise and anxiety.
Epiglottitis occurs more often in children aged 2 to 12 years, mostly boys. The main danger posed by inflammation of the epiglottis is the possibility of suffocation, therefore, at the first symptoms of the disease, you should immediately consult a doctor. There are acute and chronic inflammation of the epiglottis. If an acute form of pathology has developed, the child should be urgently taken to the hospital, transportation should be done in a sitting position.
Treatment consists of antibiotic therapy and maintaining the patency of the upper respiratory tract. If life-threatening symptoms fail, a tracheotomy is performed.
Rhinopharyngitis
Inflammation of the nasopharynx, which occurs when the throat and nose is affected by a virus, is called nasopharyngitis. Symptoms of inflammation of the nasopharynx:
- nasal congestion, as a result, difficulty breathing;
- acute sore throat, burning;
- difficulty in swallowing;
- nasality of voice;
- temperature rise.
 Children endure the inflammatory process in the nasopharynx more difficult than adults. Often, the focus of inflammation from the nasopharynx spreads to auricle leading to acute pain in the ear. Also, when the infection descends into the lower respiratory tract, the symptoms are accompanied by cough, hoarseness.
Children endure the inflammatory process in the nasopharynx more difficult than adults. Often, the focus of inflammation from the nasopharynx spreads to auricle leading to acute pain in the ear. Also, when the infection descends into the lower respiratory tract, the symptoms are accompanied by cough, hoarseness.
On average, the course of the disease of the nasopharynx lasts up to seven days, with proper treatment, rhinopharyngitis does not take a chronic form. Therapy is designed to eliminate painful symptoms. If the infection is caused by a bacterium, antibacterial drugs, in case of viral damage - anti-inflammatory drugs. It is also necessary to wash the nose with special solutions and take antipyretics if necessary.
Diseases of the larynx include acute and chronic laryngitis. acute form pathology, rarely develops in isolation, more often laryngitis becomes a consequence respiratory disease. In addition, acute laryngitis can develop as a result of:
- hypothermia;
- with a long stay in a dusty room;
- as a result of an allergic reaction to chemical agents;
- the result of smoking and drinking alcoholic beverages;
- professional overload vocal cords(teachers, actors, singers).
Symptoms of such a disease of the larynx as laryngitis are characterized by:

Acute laryngitis with voice rest and the necessary treatment disappears within 7-10 days. If the doctor's recommendations regarding treatment are not followed, the symptoms of the disease do not go away, and the laryngitis itself becomes chronic. For laryngitis it is recommended:
- alkaline inhalations;
- voice rest;
- warm drink;
- antitussive drugs;
- antiviral and immunomodulating agents;
- antihistamines for severe swelling;
- gargling;
- hot foot baths, to drain blood from the larynx and reduce its swelling, etc.
Pharyngitis
Diseases of the pharynx are most often expressed in the form of pharyngitis. This infectious pathology often develops against the background of a viral or bacterial lesion of the upper respiratory tract. Isolated pharyngitis occurs as a result of direct exposure to the pharyngeal mucosa of the irritant. For example, when talking for a long time in cold air, eating too cold or, conversely, hot food, as well as smoking and drinking alcohol.
Symptoms of pharyngitis are as follows:
- sore throat;
- pain when swallowing saliva;
- feeling of abrasion;
- pain in the ear when swallowing.
Visually, the mucous membrane of the pharynx is hyperemic, in places there may be an accumulation of purulent secretion, the tonsils are enlarged and covered with a whitish coating. Acute pharyngitis is important to differentiate from catarrhal angina. Treatment is mainly local in nature: 
- gargling;
- inhalation;
- compresses on the neck;
- absorbable lozenges for sore throats.
Chronic pharyngitis develops from acute, as well as against the background of chronic tonsillitis, sinusitis, dental caries, etc.
Diseases of the pharynx can be expressed in the form of a sore throat. Inflammation of the lymphoid tissue of the tonsils is called tonsillitis or tonsillitis. Like other diseases of the pharynx, tonsillitis can be acute or chronic. Especially often and acutely occurs pathology in children.
 The cause of tonsillitis are viruses and bacteria, mainly the following: staphylococcus aureus, streptococcus, pneumococcus, fungi of the genus Candida, anaerobes, adenoviruses, influenza viruses.
The cause of tonsillitis are viruses and bacteria, mainly the following: staphylococcus aureus, streptococcus, pneumococcus, fungi of the genus Candida, anaerobes, adenoviruses, influenza viruses.
Secondary angina develops against the background of other acute infectious processes, for example, measles, diphtheria or tuberculosis. Symptoms of angina begin acutely, they are similar to pharyngitis, but have certain differences. The tonsils greatly increase in volume, are painful to the touch, depending on the form of tonsillitis, are covered with a purulent coating or their lacunae are filled with purulent contents. Cervical lymph nodes are enlarged and may be tender to pressure. Body temperature rises to 38-39 degrees. There is pain in the throat when swallowing and perspiration.
The classification of tonsillitis is quite extensive, the following forms are distinguished:
- catarrhal - there is a superficial lesion of the tonsils. the temperature rises slightly, in the range of 37-37.5 degrees. Intoxication is not strong;
- lacunar, tonsils are covered with a yellowish-white coating, lacunae contain a purulent secretion. Inflammatory process does not spread beyond the lymphoid tissue;
- follicular, bright scarlet tonsils, edematous, festering follicles are diagnosed in the form of whitish-yellowish formations;
- phlegmonous form, more often a complication of previous types of tonsillitis. Not only the tonsils are affected, but also the peri-almond tissue. The pathology proceeds acutely, with sharp pain, more often an abscess occurs on one side. Regarding the treatment, an opening of the purulent sac and further antibiotic therapy is required.
Treatment is mainly medical, antibacterial and local effects on the mucous membrane of the pharynx. In cases where the pathology becomes chronic, systematically recurrent tonsillitis or the presence of an abscess, these are indications for the removal of the tonsils. Surgical excision of lymphoid tissue is resorted to in extreme cases, if drug therapy does not bring proper results.
Adenoid vegetations
Adenoids - a hypertrophy of the nasopharyngeal tonsil, occurs in the nasopharynx. It is most often diagnosed in children between 2 and 12 years of age. As a result of the growth of adenoid vegetation, nasal breathing is blocked and nasality of the voice occurs, with prolonged presence of adenoids, hearing loss occurs. Hypertrophy of the nasopharyngeal tonsil has three stages, the second and third are not amenable to drug treatment and requires surgical intervention - adenotomy.
Foreign bodies in the larynx or pharynx
The reason for the ingress of a foreign body into the throat is most often inattention or haste while eating. Children, left without parental supervision, may try to swallow various small objects, for example, parts from toys.
Such situations can be extremely dangerous, it all depends on the shape and size of the foreign object. If an object gets into the larynx and partially blocks its lumen, there is a danger of suffocation. Symptoms that a person is choking are:

This situation calls for urgent medical care to the victim. Emergency help must be provided immediately, otherwise there is a high risk of suffocation.
Cancer of the throat or larynx
Diseases of the pharynx can be different, but the most terrible and certainly life-threatening is cancer. Malignant growth in the pharynx or larynx, on early stages may not manifest itself in any way, which leads to late diagnosis and, accordingly, the appointment of therapy untimely. Symptoms of a tumor in the larynx are:
- not passing sensation of a foreign body in the larynx;
- desire to cough up, interfering object;
- hemoptysis;
- constant pain in the pharynx;
- breathing difficulties when the tumor is large;
- dysphonia and even aphonia, with the localization of education near the vocal cords;
- general weakness and disability;
- lack of appetite;
- weight loss.
Cancer is extremely life-threatening and has a poor prognosis. Treatment for laryngeal cancer is prescribed depending on the stage of the pathology. The main method is surgery and removal of a malignant tumor. Radiation and chemotherapy are also used. Prescribing one or another method of treatment is purely individual.
Each disease, regardless of the complexity of the course, requires attention. You should not self-medicate, and even more so, self-diagnose. Pathology can be much more complicated than you think. Timely diagnosis and the implementation of all doctor's prescriptions, allows you to achieve complete recovery and the absence of complications.